Deciding if a child has ADHD is a process with several steps. This page gives you an overview of how ADHD is diagnosed. There is no single test to diagnose ADHD, and many other problems, like sleep disorders, anxiety, depression, and certain types of learning disabilities, can have similar symptoms.
If you are concerned about whether a child might have ADHD, the first step is to talk with a healthcare provider to find out if the symptoms fit the diagnosis. The diagnosis can be made by a mental health professional, like a psychologist or psychiatrist, or by a primary care provider, like a pediatrician.
The American Academy of Pediatrics (AAP) recommends that healthcare providers ask parents, teachers, and other adults who care for the child about the child’s behavior in different settings, like at home, school, or with peers. Read more about the recommendations.
The healthcare provider should also determine whether the child has another condition that can either explain the symptoms better, or that occurs at the same time as ADHD. Read more about other concerns and conditions.

How is ADHD diagnosed?
Healthcare providers use the guidelines in the American Psychiatric Association’s Diagnostic and Statistical Manual, Fifth edition (DSM-5)1, to help diagnose ADHD. This diagnostic standard helps ensure that people are appropriately diagnosed and treated for ADHD. Using the same standard across communities can also help determine how many children have ADHD, and how public health is impacted by this condition.
Here are the criteria in shortened form. Please note that they are presented just for your information. Only trained healthcare providers can diagnose or treat ADHD.Need help?
Get information and support from the National Resource Center on ADHDexternal icon
DSM-5 Criteria for ADHD
People with ADHD show a persistent pattern of inattention and/or hyperactivity–impulsivity that interferes with functioning or development:
- Inattention: Six or more symptoms of inattention for children up to age 16 years, or five or more for adolescents age 17 years and older and adults; symptoms of inattention have been present for at least 6 months, and they are inappropriate for developmental level:
- Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or with other activities.
- Often has trouble holding attention on tasks or play activities.
- Often does not seem to listen when spoken to directly.
- Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., loses focus, side-tracked).
- Often has trouble organizing tasks and activities.
- Often avoids, dislikes, or is reluctant to do tasks that require mental effort over a long period of time (such as schoolwork or homework).
- Often loses things necessary for tasks and activities (e.g. school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones).
- Is often easily distracted
- Is often forgetful in daily activities.
- Hyperactivity and Impulsivity: Six or more symptoms of hyperactivity-impulsivity for children up to age 16 years, or five or more for adolescents age 17 years and older and adults; symptoms of hyperactivity-impulsivity have been present for at least 6 months to an extent that is disruptive and inappropriate for the person’s developmental level:
- Often fidgets with or taps hands or feet, or squirms in seat.
- Often leaves seat in situations when remaining seated is expected.
- Often runs about or climbs in situations where it is not appropriate (adolescents or adults may be limited to feeling restless).
- Often unable to play or take part in leisure activities quietly.
- Is often “on the go” acting as if “driven by a motor”.
- Often talks excessively.
- Often blurts out an answer before a question has been completed.
- Often has trouble waiting their turn.
- Often interrupts or intrudes on others (e.g., butts into conversations or games)
In addition, the following conditions must be met:
- Several inattentive or hyperactive-impulsive symptoms were present before age 12 years.
- Several symptoms are present in two or more settings, (such as at home, school or work; with friends or relatives; in other activities).
- There is clear evidence that the symptoms interfere with, or reduce the quality of, social, school, or work functioning.
- The symptoms are not better explained by another mental disorder (such as a mood disorder, anxiety disorder, dissociative disorder, or a personality disorder). The symptoms do not happen only during the course of schizophrenia or another psychotic disorder.
Based on the types of symptoms, three kinds (presentations) of ADHD can occur:
- Combined Presentation: if enough symptoms of both criteria inattention and hyperactivity-impulsivity were present for the past 6 months
- Predominantly Inattentive Presentation: if enough symptoms of inattention, but not hyperactivity-impulsivity, were present for the past six months
- Predominantly Hyperactive-Impulsive Presentation: if enough symptoms of hyperactivity-impulsivity, but not inattention, were present for the past six months.
Because symptoms can change over time, the presentation may change over time as well.
Diagnosing ADHD in Adults
ADHD often lasts into adulthood. To diagnose ADHD in adults and adolescents age 17 years or older, only 5 symptoms are needed instead of the 6 needed for younger children. Symptoms might look different at older ages. For example, in adults, hyperactivity may appear as extreme restlessness or wearing others out with their activity.
For more information about diagnosis and treatment throughout the lifespan, please visit the websites of the National Resource Center on ADHDexternal icon and the National Institutes of Mental Healthexternal icon.
Reference
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th edition. Arlington, VA., American Psychiatric Association, 2013.
Signs and Symptoms
It is normal for children to have trouble focusing and behaving at one time or another. However, children with ADHD do not just grow out of these behaviors. The symptoms continue, can be severe, and can cause difficulty at school, at home, or with friends.
A child with ADHD might:
- daydream a lot
- forget or lose things a lot
- squirm or fidget
- talk too much
- make careless mistakes or take unnecessary risks
- have a hard time resisting temptation
- have trouble taking turns
- have difficulty getting along with others
Get information and support from the National Resource Center on ADHDexternal icon
Types
There are three different types of ADHD, depending on which types of symptoms are strongest in the individual:
- Predominantly Inattentive Presentation: It is hard for the individual to organize or finish a task, to pay attention to details, or to follow instructions or conversations. The person is easily distracted or forgets details of daily routines.
- Predominantly Hyperactive-Impulsive Presentation: The person fidgets and talks a lot. It is hard to sit still for long (e.g., for a meal or while doing homework). Smaller children may run, jump or climb constantly. The individual feels restless and has trouble with impulsivity. Someone who is impulsive may interrupt others a lot, grab things from people, or speak at inappropriate times. It is hard for the person to wait their turn or listen to directions. A person with impulsiveness may have more accidents and injuries than others.
- Combined Presentation: Symptoms of the above two types are equally present in the person.
Because symptoms can change over time, the presentation may change over time as well.“Is It ADHD?” in ASLhttps://www.youtube-nocookie.com/embed/GRA3ZbCiBzc?autohide=0&enablejsapi=1&playerapiid=37055&modestbranding=1&rel=0&origin=https://www.cdc.gov&showinfo=0//www.youtube-nocookie.com/embed/GRA3ZbCiBzc?autohide=0&enablejsapi=1&playerapiid=37055&modestbranding=1&rel=0&origin=https://www.cdc.gov&showinfo=0&wmode=opaque?enablejsapi=1txt iconAudio Descriptionmedia iconLow Resolution Video
american sign language interpreting icon Learn about symptoms of ADHD, how ADHD is diagnosed, and treatment recommendations including behavior therapy, medication, and school support.
Causes of ADHD
Scientists are studying cause(s) and risk factors in an effort to find better ways to manage and reduce the chances of a person having ADHD. The cause(s) and risk factors for ADHD are unknown, but current research shows that genetics plays an important role. Recent studies of twins link genes with ADHD.1
In addition to genetics, scientists are studying other possible causes and risk factors including:
- Brain injury
- Exposure to environmental (e.g., lead) during pregnancy or at a young age
- Alcohol and tobacco use during pregnancy
- Premature delivery
- Low birth weight
Research does not support the popularly held views that ADHD is caused by eating too much sugar, watching too much television, parenting, or social and environmental factors such as poverty or family chaos. Of course, many things, including these, might make symptoms worse, especially in certain people. But the evidence is not strong enough to conclude that they are the main causes of ADHD.ADHD Fact Sheet

Download and Print this fact sheet pdf icon[PDF – 473 KB]
Diagnosis
Deciding if a child has ADHD is a process with several steps. There is no single test to diagnose ADHD, and many other problems, like anxiety, depression, sleep problems, and certain types of learning disabilities, can have similar symptoms. One step of the process involves having a medical exam, including hearing and vision tests, to rule out other problems with symptoms like ADHD. Diagnosing ADHD usually includes a checklist for rating ADHD symptoms and taking a history of the child from parents, teachers, and sometimes, the child.
Learn more about the criteria for diagnosing ADHD
Treatments

In most cases, ADHD is best treated with a combination of behavior therapy and medication. For preschool-aged children (4-5 years of age) with ADHD, behavior therapy, particularly training for parents, is recommended as the first line of treatment before medication is tried. What works best can depend on the child and family. Good treatment plans will include close monitoring, follow-ups, and making changes, if needed, along the way.
Managing Symptoms: Staying Healthy
Being healthy is important for all children and can be especially important for children with ADHD. In addition to behavioral therapy and medication, having a healthy lifestyle can make it easier for your child to deal with ADHD symptoms. Here are some healthy behaviors that may help:
- Developing healthy eating habits such as eating plenty of fruits, vegetables, and whole grains and choosing lean protein sources
- Participating in daily physical activity based on age
- Limiting the amount of daily screen time from TVs, computers, phones, and other electronics
- Getting the recommended amount of sleep each night based on age
Get Help!
If you or your doctor has concerns about ADHD, you can take your child to a specialist such as a child psychologist or developmental pediatrician, or you can contact your local early intervention agency (for children under 3) or public school (for children 3 and older).
The Centers for Disease Control and Prevention (CDC) funds the National Resource Center on ADHDexternal icon, a program of CHADD – Children and Adults with Attention-Deficit/Hyperactivity Disorder. Their website has links to information for people with ADHD and their families. The National Resource Center operates a call center (1-866-200-8098) with trained staff to answer questions about ADHD.
For more information on services for children with special needs, visit the Center for Parent Information and Resources.external icon To find the Parent Center near you, you can visit this website.external icon
ADHD in Adults
ADHD can last into adulthood. Some adults have ADHD but have never been diagnosed. The symptoms can cause difficulty at work, at home, or with relationships. Symptoms may look different at older ages, for example, hyperactivity may appear as extreme restlessness. Symptoms can become more severe when the demands of adulthood increase. For more information about diagnosis and treatment throughout the lifespan, please visit the websites of the National Resource Center on ADHDexternal icon and the National Institutes of Mental Healthexternal icon.
What is disability?
A disability is any condition of the body or mind (impairment) that makes it more difficult for the person with the condition to do certain activities (activity limitation) and interact with the world around them (participation restrictions).
There are many types of disabilities, such as those that affect a person’s:
- Vision
- Movement
- Thinking
- Remembering
- Learning
- Communicating
- Hearing
- Mental health
- Social relationships
Although “people with disabilities” sometimes refers to a single population, this is actually a diverse group of people with a wide range of needs. Two people with the same type of disability can be affected in very different ways. Some disabilities may be hidden or not easy to see.
According to the World Health Organization, disability has three dimensions:1
- Impairment in a person’s body structure or function, or mental functioning; examples of impairments include loss of a limb, loss of vision or memory loss.
- Activity limitation, such as difficulty seeing, hearing, walking, or problem solving.
- Participation restrictions in normal daily activities, such as working, engaging in social and recreational activities, and obtaining health care and preventive services.
Disability can be:
- Related to conditions that are present at birth and may affect functions later in life, including cognition (memory, learning, and understanding), mobility (moving around in the environment), vision, hearing, behavior, and other areas. These conditions may be
- Disorders in single genes (for example, Duchenne muscular dystrophy);
- Disorders of chromosomes (for example, Down syndrome); and
- The result of the mother’s exposure during pregnancy to infections (for example, rubella) or substances, such as alcohol or cigarettes.
- Associated with developmental conditions that become apparent during childhood (for example, autism spectrum disorder and attention-deficit/hyperactivity disorder or ADHD)
- Related to an injury (for example, traumatic brain injury or spinal cord injuryexternal icon).
- Associated with a longstanding condition (for example, diabetes), which can cause a disability such as vision loss, nerve damage, or limb loss.
- Progressive (for example, muscular dystrophy), static (for example, limb loss), or intermittent (for example, some forms of multiple sclerosisexternal icon).
Related Health Conditions
The following links provide information from CDC’s National Center on Birth Defects and Developmental Disabilities on certain disability-related health conditions:
- Attention-Deficit / Hyperactivity Disorder (ADHD)
- Autism
- Cerebral Palsy
- Deep Vein Thrombosis (DVT) (Blood Clots)
- Duchenne/Becker Muscular Dystrophy
- Fetal Alcohol Spectrum Disorders (FASD)
- Fragile X Syndrome
- Hearing Loss
- Hemophilia
- Intellectual Disability
- Kernicterus
- Sickle Cell Disease
- Spina Bifida
- Thalassemia
- Tourette Syndrome
- Traumatic Brain Injury
- Vision Impairment
- Von Willebrand Disease
What is impairment?
Impairment is an absence of or significant difference in a person’s body structure or function or mental functioning.2 For example, problems in the structure of the brain can result in difficulty with mental functions, or problems with the structure of the eyes or ears can result in difficulty with the functions of vision or hearing.
- Structural impairments are significant problems with an internal or external component of the body. Examples of these include a type of nerve damage that can result in multiple sclerosisexternal icon, or a complete loss of a body component, as when a limb has been amputated.
- Functional impairments include the complete or partial loss of function of a body part. Examples of these include pain that doesn’t go away or joints that no longer move easily.
What is the difference between activity limitation and participation restriction?
The World Health Organization (WHO) published the International Classification of Functioning, Disability and Health (ICF) in 2001. The ICF provides a standard language for classifying body function and structure, activity, participation levels, and conditions in the world around us that influence health. This description helps to assess the health, functioning, activities, and factors in the environment that either help or create barriers for people to fully participate in society.
According to the ICF:
- Activity is the execution of a task or action by an individual.
- Participation is a person’s involvement in a life situation.
The ICF acknowledges that the distinction between these two categories is somewhat unclear and combines them, although basically, activities take place at a personal level and participation involves engagement in life roles, such as employment, education, or relationships. Activity limitations and participation restrictions have to do with difficulties an individual experiences in performing tasks and engaging in social roles. Activities and participation can be made easier or more difficult as a result of environmental factors, such as technology, support and relationships, services, policies, or the beliefs of others.
The ICF includes the following in the categories of activities and participation:
- Learning and applying knowledge
- Managing tasks and demands
- Mobility (moving and maintaining body positions, handling and moving objects, moving around in the environment, moving around using transportation)
- Managing self-care tasks
- Managing domestic life
- Establishing and managing interpersonal relationships and interactions
- Engaging in major life areas (education, employment, managing money or finances)
- Engaging in community, social, and civic life
It is very important to improve the conditions in communities by providing accommodations that decrease or eliminate activity limitations and participation restrictions for people with disabilities, so they can participate in the roles and activities of everyday life.
References
- World Health Organization, International Classification of Functioning, Disability and Health (ICF)external icon. Geneva: 2001, WHO.
- US Department of Health and Human Services. The Surgeon General’s Call to Action to Improve the Health and Wellness of Persons with Disabilitiesexternal icon. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2005.
Your odds of becoming disabled before you retire are about 1 in 3. And some of the causes of disability might surprise you. Some conditions that cause people to miss work include:
Here’s a closer look at some of the most common disabling conditions — and some tips on how to protect yourself from the high medical bills that may come with them.
Common Conditions That Cause Disability
Arthritis and other musculoskeletal problems. These are the most common causes of long-term disability. They make up as much as a third of all disability cases. Arthritis is probably the biggest single cause.
About 1 in 3 people say arthritis affects their ability to do their jobs in some way, according to the CDC.
Other muscle and joint problems — bad backs, bones that never mend, bad hips — are common causes of disability too, says Matt Tassey. He’s a former chairman of the nonprofit Life and Health Insurance Foundation for Education (LIFE).
Heart disease and stroke. People may live with heart disease for years or decades. It can severely limit their ability to work. Studies estimate that heart disease is now the reason for 17% of all health costs in the U.S.
Cancer. While cancer itself can be disabling, treatments such as surgery, radiation, and chemotherapy can also make it difficult to work.
“Cancer is the fastest-growing cause for disability claims,” Tassey says. Why? In part, this reflects a rising rate of cancer, he says. It could also result from more effective treatment. “We’re doing medical miracles today,” he says. “People are living much longer after a cancer diagnosis than they once did.”
Mental health problems. You might think of disability as physical, but mental health problems can make work difficult or impossible. Depression, bipolar disorder, and other conditions can be as disabling as any physical illness.
Mental health problems are the most common reason that people file for Social Security disability, Tassey says.
Diabetes. As a cause of disability, diabetes is rising fast, Tassey says. Along with obesity, it’s linked to a number of serious health problems, like heart disease.
Behavior modification is a complex term that has different meanings for different professionals. For some, it refers to techniques that are coercive or intended to create pain. CPI strongly opposes treatment modalities that adversely affect a person’s Care, Welfare, Safety, and Security℠ and does not teach behavior modification. Rather, we teach safe, noninvasive, and nonharmful behavior management skills for crisis prevention and intervention. Our training is entrenched in helping you positively interact with and support the individuals in your care.
As such, if you’re looking for safe strategies that won’t cause harm and that will effectively prevent and stop difficult behavior, we can help you center your care on positive techniques that ensure safety for yourself, your staff, and the individuals you support.
4 Strategies for Promoting Positive Change
Behavior management skills that are positive and not punitive involve viewing not the person as a problem, but the environment and the skill deficiencies as factors that require change. The goal is not to modify the person, but to modify the setting, to personalize your approach, and to help the person build skills and relationships. Here are four strategies for effecting positive change.
- Be Mindful of Your Own Behavior.
One vital aspect of crisis intervention to keep in mind is that while you cannot change an individual’s behavior, you can modify your own approach, as your behavior affects the individual’s behavior and vice versa. How you react in a situation influences the behaviors and events that follow. - Remember That Behavior Is Communication.
Another important consideration is that behavior is communication. With any behavior, an individual wants to be understood, to be treated with respect, and to satisfy her needs. When you understand the underlying causes of difficult behaviors and empower an individual with the choice of replacing problem behaviors with positive behaviors that meet the same needs, you’re better able to guide her toward expressing herself in a positive way. - Adapt the Environment.
A key to preventing difficult behavior is lessening or eliminating the environmental triggers that cause an individual to feel anxiety. Whether the individual is a student in a classroom, a patient in a hospital, or a client in a residential setting, help him organize and modify his environment in a way that works for him. Making caring and respectful modifications to the factors that cause him to act out is an essential part of developing a safe behavior management program that supports positive conduct. For instance, if a person in your care is sensitive to fluorescent lights, meet his sensory needs with natural or incandescent light. If you have a student who feels anxious at the sound of loud or sudden noise, ask her if she would be more comfortable positioned away from the door or the hallway. - Build Rapport.
When you have strong relationships with the individuals in your care, you can get to the root of their behavior and help them make positive change. Very often, what needs modification is not the individual himself, but the factors that cause him to act out. Therefore, understanding the individual’s likes, needs, and wishes is central to creating an environment that is positive and maintains the person’s dignity. When you connect with someone with empathy and compassion, that person will feel respected—and his disruptive behavior will de-escalate as a result. He will respond positively when you show him that you care and that you know how to safely and respectfully guide him from chaos to calm.
Behavior Modification Techniques Resources
Our free eBook, Creating a Safe and Caring Work Environment, is packed with effective strategies for safely preventing and stopping anxiety and disruption. Download this helpful resource and get safe and respectful tips for preventing problem behavior and effecting positive behavior change. When you’re equipped with these useful tips and the evidence-based strategies presented in our Nonviolent Crisis Intervention® training program, you and your staff will be better able to stop problems and foster harmony. Keep in mind that while you can’t force anyone to do anything, you can guide individuals toward behavior that is both positive and centered on safety and respect!
The following articles contain a wealth of techniques for safely and effectively supporting positive behavior. Modification of the factors that cause difficult behavior is emphasized. Please note that while CPI does not endorse the external resources, we believe that they may be helpful to you in your efforts to empower individuals to express themselves in positive ways.
These resources, which focus on behavior management rather than behavior modification, are ranked alphabetically.
- The Benefits of Empathic Listening—Learn more about how active listening builds rapport and trust.
- Building a Better Behavioral Framework: Tiers of Positive School Support—Find out about the Wauwatosa School District’s success with building positive relationships, boosting behavioral and academic achievement, and decreasing disciplinary issues.
- Expecting the Unexpected: Responding to Unpredictable Behavior—CPI president Judith Schubert discusses the impact of trauma and drug use on behavior and outlines six strategies for intervention.
- PBIS.org—Access numerous resources about implementing Positive Behavioral Interventions and Supports (PBIS).
- Positive Behavior Support and the Nonviolent Crisis Intervention® Training Program—Get the Top 10 PBIS Online Resources, view a free webinar, access information about how our training corresponds with PBIS principles, and more.
- Preventing Problematic Behaviors: It Starts With Staff Training—CPI’s Dr. Randy Boardman, executive director of research and development, explains how professional development and training can help decrease problematic behavior in schools.
- Responding to Aggressive Behavior: Impact of Training on Staff Members’ Knowledge and Confidence—Learn more about how training improves staff’s ability to safely handle disruptive behavior.
- Taking the Trauma Out of Security—Find out how security and psychiatric nursing staff at Baystate Medical Center (BMC) calmed tensions and fostered cooperation with a staff training program.
Access additional articles, eBooks, webinars, and other
IntroductionDefinition:
Male sex hormones are group of steroid hormones called androgens. Androgens are hormones responsible for the male features and reproduction. Some are naturally produced in the body, and if the body doesn’t make them properly, they can be obtained through prescription medication. Androgens are responsible for sexual development in males and are produced by the testes. Women have smaller amounts of androgens too, and the ovaries produce them. The most well-known is probably testosterone.
3-
»
Hormones, like androgens, facilitate communication between cells around the entire body. Some cells have androgen receptors. Think of each hormone as a key and receptors as a lock—together they make your body systems work. Hormones created from cholesterol, like androgens, are known as steroid hormones.
Androgens are produced in the adrenal gland and the ovaries through the conversion of cholesterol. Muscle and fat tissue can also synthesize testosterone.
Importance:
Androgens don’t just impact sexual health; they also play a role in metabolism, insulin sensitivity, and possibly body composition (the amount and distribution of body fat and muscle).
Androgens may also impact bone density and cardiovascular health in cis-gender women, and some research suggests that they may have an impact on brain function and mood, but more research is needed.
Testosterone is not only important for males, androgens generally and testosterone specifically have serious role in females:
The most important progesterone, estradiol, is actually synthesized from testosterone by an enzyme called aromatase. Androgens also appear to impact the function of the endometrium (the lining of the uterus), and may play a role in helping prepare it to
support a potential pregnancy.
Types & Sourcesv Androgens are classified into natural or synthetic
–
4-
Ø
Natural androgens:
These are the androgens naturally occurring in male or female body which are:
- Testosterone
- Dehydrotestosteron(DHT) {more active derivative of testosterone by 5α-reductase)
- Weaker androgens
• Dehydroepiandrosteron(DHEA)
• Androstenedione - Androsterone (execratory form)
• Testes of adult male produce 5–12 mg of testosterone daily, a part of which is converted in extra glandular tissues to the more active dihydrotestosterone (DHT); by the enzyme steroid 5 α-reductase; cholesterol is the starting material and the same pathway is utilized.
• Adrenal cortex produces small quantities of dehydroepiandrosterone(DHEA) and androstenedione which are called ‘weak androgens’ (potency 1/20 to 1/30), but are in fact inactive as such and derive their weak activity from partial conversion to testosterone in peripheral tissues. Adrenals themselves do not produce significant quantity of testosterone.
• In women ovary produces small quantity of testosterone; this together with that derived indirectly from adrenals amounts to 0.25–0.5 mg/day.
• Androsterone It is a metabolite of testosterone which is excreted in urine. It has 1/10 the activity of testosterone.
Ø Synthetic androgens:
This group include the androgens that have been developed outside the body to be used as androgen replacement therapy.
Synthetic androgens include both steroidal and nonsteroidal androgens. Synthetic steroidal androgens, most developed by 1970, comprise categories of: - 17α-alkylated androgens, (methyltestosterone, fluoxymesterone, oxymetholone, oxandrolone, ethylestrenol, stanozolol, danazol, methandrostenolone, norethandrolone)
- 1-methyl androgen
– Nandrolone and its derivatives.
5-
v Source of male sex hormones:
a) Testosterone
Like other steroid hormones, testosterone is derived from cholesterol.
The largest amounts of testosterone (>95%) are produced by the testes in men, while the adrenal glands account for most of the remainder. Testosterone is also synthesized in far smaller total quantities in women by the adrenal glands, thecal cells of
the ovaries, and, during pregnancy, by the placenta. In the testes, testosterone is produced by the Leydig cells.] The male generative glands also contain Sertoli cells, which require testosterone for spermatogenesis. Like most hormones, testosterone is supplied to target tissues in the blood where much of it is transported bound to a specific plasma protein, sex hormone-binding globulin (SHBG).
b) Androgens
The main subset of androgens, known as adrenal androgens, is composed of 19- carbon steroids synthesized in the zona reticularis, the innermost layer of the adrenal cortex. Adrenal androgens function as weak steroids (though some are precursors),
and the subset includes dehydroepiandrosterone (DHEA), dehydroepiandrosterone sulfate (DHEA-S), androstenedione (A4), and androstenediol (A5).
Besides testosterone, other androgens include:
-6-
1- Dehydroepiandrosterone (DHEA): is a steroid hormone produced in the adrenal cortex from cholesterole t is the primary precursor of natural estrogens. DHEA is also called dehydroisoandrosterone or dehydroandrosterone.
2-Androstenedione:is an androgenic steroid produced by the testes, adrenal cortex, and ovaries. While androstenediones are converted metabolically
to testosterone and other androgens, they are also the parent structure of estrone. Use of androstenedione as an athletic or bodybuilding supplement has been banned by the International Olympic Committee, as well as other sporting organizations.
3-Androstenediol: is the steroid metabolite thought to act as the main regulator of gonadotropin secretion
4-Androsterone: is a chemical byproduct created during the breakdown of androgens, or derived from progesterone, that also exerts minor masculinising effects, but with one-seventh the intensity of testosterone. It is found in approximately equal amounts in the plasma and urine of both males and females.
5-Dihydrotestosterone (DHT): is a metabolite of testosterone, and a more potent androgen than testosterone in that it binds more strongly to androgen receptors. It is produced in the skin and reproductive tissue.
-7-
»
Preparations
Androgens are synthetically modified to make drugs used for both men and women which is called Androgen replacement therapy (ART), often referred to as testosterone replacement therapy (TRT), is a form of hormone therapy in which androgens, often testosterone, are replaced. ART is often prescribed to counter the effects of male hypogonadism. It typically involves the administration of testosterone through:
Injections
skin creams patches
gels
subcutaneous pellets
•
Modifications
injectable testosterone, an “ester” functional group is usually added to the
testosterone molecule (see Figure 3, below). There are many different ester
groups that can be added to testosterone: (cypionate, enanthate, acetate,
propionate, phenylpropionate, isocaproate, caproate, decanoate, and
undecanoate.)
Ester groups are added to improve the solubility of testosterone in oil, which in turn
slows the release of the testosterone from its injection site into the blood stream.
Without an added ester group, injectable testosterone would enter the blood
stream very quickly, and would have to be administered in small doses daily (or
several times a day) in order to maintain acceptable levels of the hormone in the
body. Thus, adding an ester group to an injectable allows for a relatively easy
–
dosing regimen, far fewer shots, and a slow release of hormone into the system.
“esterase enzymes” in a process known as “hydrolization.” Once the ester group
has been removed by these enzymes, the testosterone is returned to its
As a testosterone ester enters the blood stream, the ester group is cleaved off by
-“bioidentical” form, thus making it bioavailable and ready to perform its various
actions and effects.
e to do its work in the body.
The use of methylated testosterone did have the result of making oral testosterone more readily bioavailable, but it also was found to be very hard on the liver, and thus caused health problems. Because of this, methyltestosterone is rarely used for hormone therapy today, as safer forms of delivery have become available.
A more recent development in oral testosterone delivery is the use of a capsule form of testosterone (undecanoate), a testosterone ester dissolved in oleic acid. Because it is designed to be absorbed through the small intestine into the lymphatic system (thus circumventing the “first pass” through the liver), it poses less burden on the liver than methyltestosterone. Therefore, it is considered a safer oral form of testosterone.
8-
orally, modifications have been made to the testosterone molecule to try to combat
problems caused by the “first pass effect.” Drugs that are taken orally (i.e.,
swallowed) are absorbed from the gastrointestinal tract and pass via the portal
vein into the liver. If bioidentical testosterone is given orally, a very large portion is
metabolized during this “first pass” through the liver, and therefore it cannot
become bioavailabl
–
Ø Transdermal (i.e., medication is absorbed through the skin)
bioidentical testosterone becomes active quickly once absorbed through the skin,
it must be applied daily to maintain appropriate levels of testosterone in the body. Depending on the formulation, transdermal preparations might also include additional ingredients to accelerate the absorption of the testosterone through the skin. Some of these ingredients can cause side effects, such as rashes and skin irritation. Transdermal testosterone is available in both brand-name and compounded preparations; a prescription for compounded transdermal testosterone can be tailored by your doctor for your specific dosage requirement
Ø Sublingual/buccal
Sublingual and buccal testosterone treatments, which are dissolved in the mouth rather than swallowed, are generally made with bioidentical testosterone. Sublingual preparations are dissolved under the tongue; these can be prepared by compounding pharmacies. Buccal testosterone delivery works placing a tablet against the surface of the gums. Buccal testosterone systems are available as name-brand or compounded preparations. Sublingual/buccal delivery is different
-from oral delivery in that very little of the substance is swallowed, avoiding potential “first pass effect” problems with the liver. Because bioidentical testosterone is absorbed quickly through sublingual/buccal routes, it must be applied more than once a day to maintain appropriate levels of testosterone in the body.
Ø Subcutaneous pellet
Subcutaneous testosterone pellets are made of bioidentical, crystalline testosterone that is implanted beneath the skin. The pellets are about the size of a grain of rice, and are typically placed in the buttocks or abdomen by a doctor. Because of their crystalline form, the testosterone in subcutaneous pellets is released slowly over a period of weeks or months.
9-
-10 –
Pharmacokinetics
Testosterone
The pharmacokinetics of testosterone, including
its bioavailability, metabolism, biological half-life, and other parameters, differ by route of administration. Likewise, the potency of testosterone, and its local effects in certain tissues, for instance the liver, differ by route of administration as well. In particular, the oral route is subject to a high first- pass effect, which results in high levels of testosterone in the liver and consequent hepatic androgenic effects, as well as low potency due to first- pass metabolism in the intestines and liver
into metabolites like dihydrotestosterone and androgen
conjugates. Conversely, this is not the case for non-oral routes, which bypass the first pass.
Different testosterone routes and dosages can achieve widely varying circulating testosterone levels.
• routes of administrations
Testosterone can be taken by a variety of different routes of administration. These include:
- oral
- buccal
- sublingual
intranasal - transdermal (gels, creams, patches, solutions)
- vaginal (creams, gels, suppositories)
- rectal (suppositories)
- injections: intramuscular or subcutaneous (in oil solutions or aqueous suspensions)
- subcutaneous implant
1- Absorption: –
11 – - The oral bioavailability of testosterone is very low. The bioavailability of oral testosterone undecanoate is 3 to 7%.
- Topical testosterone gels have a bioavailability of about 8 to 14% when administered to recommended skin sites including the abdomen, arms, shoulders, and thighs.
- The bioavailability of testosterone by subcutaneous implant is virtually 100%.The bioavailability of drugs that are administered intramuscularly is generally almost 95%
Oral administration:
Testosterone is well-absorbed but extensively metabolized with oral
administration due to the first pass through the intestines and liver. It is
rapidly and completely inactivated in men at doses of less than 200 mg. In
large doses, such as 200 mg however, significant increases in circulating
testosterone levels become apparent. In addition, while a 60 mg dose has
no effect on testosterone levels in men, this dose does measurably increase
testosterone levels in prepubertal boys and women.
The oral bioavailability of testosterone in young women after a single 25 mg
dose was found to be 3.6 ± 2.5%. but Instead of in its free unesterified form,
testosterone is used by oral administration in the form of testosterone
undecanoate. this testosterone ester
bypass a portion of first-pass
metabolism in the liver and producing measurable increases in testosterone
levels at much lower doses than free testosterone.
Buccal administration:
Mucoadhesive tablets are applied to the gums of the mouth and provide
controlled and sustained release of testosterone as the buccal system
hydrates. This system delivers testosterone directly into the systemic
circulation and bypasses the liver, avoiding first pass metabolism and –
12 –
increasing bioavailability. Each tablet contains 30 mg of testosterone and
one tablet is applied every 12 hours, alternating sides of the mouth above
the incisor teeth
Transdermal administration:
Testosterone is available for transdermal administration in the form
of gels, creams, scrotal and non-scrotal patches, and axillary solutions.
Transdermal testosterone gel has a bioavailability of about 8 to 14% when administered to recommended skin sites including
the abdomen, arms, shoulders, and thighs. Scrotal skin is the thinnest skin of the body and has enhanced absorption characteristics relative to other skin areas. Application of testosterone gels and creams to the scrotum has been studied and achieves much higher levels of testosterone than conventional skin sites. Scrotal application of testosterone requires approximately 5-fold lower doses relative to non-scrotal application.
Subcutaneous implant:
Testosterone can be administered in the form of a subcutaneous pellet
implant. The bioavailability of testosterone when administered as a
subcutaneous pellet implant is virtually 100%.
Levels of testosterone vary considerably between individuals, but are fairly
constant within individuals.The absorption half-life of subdermal
testosterone implants is 2.5 months.The replacement interval is once every
four to six months.
Intramuscular injection:
Testosterone can be administered by intramuscular injection either as
an aqueous suspension of testosterone or as an oil solution or aqueous
suspension of testosterone esters such as testosterone
propionate, testosterone enanthate, testosterone cypionate, testosterone
undecanoate, and testosterone isobutyrate. These preparations are prodrugs of progesterone that have a long-lasting depot
effect when injected
into muscle or fat, ranging from days to months in duration. The bioavailability of drugs that are administered intramuscularly is generally almost 95% –
13 –
2- Distribution:
In the circulation, 97.0 to 99.5% of testosterone is bound to plasma proteins, with 0.5 to 3.0% unbound.It is tightly bound to SHBG and weakly
to albumin.Of circulating testosterone, 30 to 44% is bound to SHBG while 54 to 68% is bound to albumin. Unlike testosterone that is bound to SHBG, bioavailable testosterone is bound to plasma proteins weakly enough such that, similarly to free testosterone,and it may be biologically active.
3- Metabolism:
Testosterone is metabolized primarily in the liver mainly (90%) by reduction via 5α- and 5β-
reductase and conjugation via glucuronidation and sulfation.The
major urinary metabolites of testosterone
are androsterone
glucuronide and etiocholanolone glucuronide.
The elimination half-life of testosterone varies depending on the route of administration and formulation and on whether or not it is esterified.The elimination half-life of testosterone in the blood or by intravenous injection is only about 10 minutes.Conversely, testosterone and testosterone esters in oil solution or crystalline aqueous
suspension administered by intramuscular or subcutaneous injection have much longer half-lives, in the range of days to months, due to slow release from the injection sites .
(less than 0.01%) is found unchanged in the urine.
4- Elimination:
Testosterone and its metabolites are eliminated in urine. It
is excreted mainly as androsterone glucuronoide and etiocholanolone glucuronide. It is also excreted to a small extent as other conjugates such as testosterone glucuronide (1%), testosterone sulfate (0.03%), and androstanediol glucuronides. Only a very small amount of testosterone
Student name:
Elsayed Naser Abd-Elrahman Yousef Anas Abd-Elbaset Abd-Elmohsen –
14 –
Pharmacodynamics
a) Mechanism of action:
1-pre-receptor activation
Androgen action involves pre-receptor, receptor and post-receptor mechanisms that are centered on the binding of testosterone (or an analog) to the androgen receptor. Testosterone undergoes pre-receptor activation by conversion to potent bioactive metabolites, DHT and estradiol. The steroidogenic enzyme 5a-reductase has two isozymes, types 1 and 2, which form a local androgen amplification mechanism converting testosterone to the most potent natural androgen, DHT. The two isozymes have different chromosomal location and distinct biochemical features but are homologous genes . They are structurally and functionally unrelated to a third 5a- reductase (SRD5A3) which may have physiological role in fatty acid rather than steroidal biochemistry . This local androgen amplification mechanism is exemplified in urogenital sinus derived tissues, notably external and internal genitalia and the prostate, which characteristically express high levels of 5a-reductase type 2. Other tissues such as non-genital skin and liver express 5a-reductase type 1. The other form of pre-receptor androgen activation is conversion of testosterone to estradiol by the enzyme aromatase, which diversifies androgen action by facilitating effects mediated via Estrogen Receptors(ER). Consequently, while DHT may be considered a pure androgen because its bioactivity is solely mediated via Androgen Receptors(AR), testosterone has a wider spectrum of action which includes diversification by aromatization and ER mediated effects. These pre-receptor mechanisms provide testosterone with a versatile and subtle range of regulatory mechanisms prior to receptor mediated effects, depending on the balance between direct AR mediated vs indirect actiational and/or ER mediated mechanisms. In addition, tissues vary in their androgenic thresholds and dose-response characteristics to testosterone and its bioactive metabolites
2-action on receptors
15 –
The biological effects of testosterone can be considered by the receptor it activates and by the tissues in which effects occur at various stages of life. Testosterone can act as:
- an androgen, either directly, by binding to the androgen receptor, or indirectly by conversion to dihydrotestosterone, which binds to the androgen receptor even more avidly than testosterone.
- an estrogen, by conversion to estradiol, which binds to the estrogen receptor
• Direct effects of testosterone and effects mediated indirectly via dihydrotestosterone or estradiol
testosterone, after conversion into DHT, is also metabolized into 3α-androstanediol,
a neurosteroid and potent positive allosteric modulator of the GABAA receptor, and 3β- androstanediol, a potent and preferential agonist of the ERβ. These metabolites, along with estradiol, may be involved in a number of the effects of testosterone in the brain, including its antidepressant, anxiolytic, stress-relieving, rewarding, and pro-
sexual effects
Effects That Occur Via the Androgen Receptor:
Testosterone and dihydrotestosterone act as androgens via a single androgen receptor
The androgen receptor officially designated NR3A is a member of the nuclear receptor superfamily (steroid hormone receptors, thyroid hormone receptors, and orphan receptors). The androgen receptor is comprised of an amino-terminal domain, a DNA-binding domain, and a ligand-binding domain. Testosterone and dihydrotestosterone bind to the ligand-binding domain, causing a conformational change in the receptor that allows the ligand-receptor complex to translocate to the nucleus and bind via the DNA-binding domain to androgen response elements on certain responsive genes. The ligand-receptor complex acts as a transcription factor complex and stimulates expression of those genes
The mechanisms by which androgens have different actions in diverse tissues have become clearer in recent years. –
• Effects That Occur Via the Estrogen Receptor:
The effects of testosterone on at least one tissue are mediated by its conversion to
estradiol, catalyzed by the CYP19 enzyme complex , In the rare cases in which a male does not express CYP19 or the estrogen receptorthe epiphyses do not fuse and long- bone growth continues indefinitely. In addition, the patients are osteoporotic. Administration of estradiol corrects the bone abnormalities in patients with CYP19 deficiency but not in those with an estrogen-receptor defect. Because men have larger bones than women, and bone cells express the androgen receptor testosterone also may have an effect on bone via the androgen receptor. Administration of estradiol to a man with CYP19 deficiency increased his libido suggesting that the effect of testosterone on male libido may be mediated by conversion to estradiol
b) Effects:
Effects in the body and brain:
16 – - One mechanism is the higher affinity with which dihydrotestosterone binds to and activates the androgen receptor compared to testosterone.
- Another mechanism involves transcription co-factors, both co-activators and co- repressors, which are tissue-specific. At this time, the roles of co-factors are better described for other nuclear receptors than for the androgen receptor
o Promotes growth, function, and maintenance of the prostate gland, seminal vesicles, and penis during puberty and thereafter
o Promotes growth and maintenance of muscles, particularly of the upper body
o Causes subcutaneous fat to be deposited in a masculine pattern and decreases
overall body fat –
17 –
o Suppresses breast development induced by estrogens, but can also still produce gynecomastia via excessive conversion into estradiol if levels are too high
o Maintains skin health, integrity, appearance, and hydration and slows the rate of aging of the skin, but can also cause oily skin, acne, and seborrhea
o Promotes the growth of facial and body hair, but can also cause scalp hair loss and hirsutism
o Contributes to bone growth and causes broadening of the shoulders at puberty
o Modulates liver protein synthesis, such as the production of sex hormone-binding
globulin and many other proteins
o Increases production of erythropoietin in the kidneys and thereby stimulates red
blood cell production in bone marrow and elevates hematocrit
o Exerts negative feedback on the hypothalamic–pituitary–gonadal axis by
suppressing the secretion of the gonadotropins follicle-stimulating
hormone (FSH) and luteinizing hormone (LH) from the pituitary gland, thereby inhibiting gonadal sex hormone production as well
as spermatogenesis and fertility
o Regulates the vasomotor system and body temperature via the hypothalamus, thereby preventing hot flashes
o Modulates brain function, with effects on mood, emotionality, aggression, and sexuality, as well as cognition and memory
o Increases sex drive and erectile capacity and causes spontaneous erections and nocturnal emissions
o Increases the risk of benign prostatic hyperplasia and prostate cancer and accelerates the progression of prostate cancer
o Decreases breast proliferation and the risk of breast cancer
Androgens are used for several reasons, such as:
18 –
• To replace the hormone when the body is unable to produce enough on its own.
• To stimulate the beginning of puberty in certain boys who are late starting puberty naturally.
• To treat certain types of breast cancer in females.
In addition, some of these medicines may be used for other conditions as determined by the doctor.
In Men
Androgen replacement is the classic treatment of hypogonadism. It is also used in men who have lost the ability to produce androgens due to disease or its treatment
Androgen replacement therapy formulations and dosages used in men show
In Diabetes
The risks of diabetes and of testosterone deficiency in men over 45 (i.e., hypogonadism, specifically hypoandrogenism) are strongly correlated. Testosterone replacement therapies have been shown to improve blood glucose management. Still, “it is prudent not to start testosterone therapy in men with diabetes solely for the purpose of improving metabolic control if they show no signs and symptoms of hypogonadism.”
In Women
Androgen replacement is used in postmenopausal women: the indications are to increase sexual desire; and to prevent or treat osteoporosis. The androgens used for androgen replacement in women include testosterone (and esters), prasterone (dehydroepiandrosterone; DHEA) (and the ester prasterone enanthate), methyltestosterone, nandrolone decanoate, and tibolone, among others.
Androgen therapy for men :
Androgen therapy can be classified as physiologic replacement or pharmacologic therapy according to the dose, type of androgen and objectives of treatment.
- Androgen replacement therapy aims to restore tissue androgen
–
–
exposure in androgen-deficient men due to pathological hypogonadism (disorders of the reproductive system) to levels comparable with those of eugonadal men. Using the natural androgen testosterone and a dose limited to one that maintains blood testosterone levels within the eugonadal range, androgen replacement therapy aims to restore the full spectrum of androgen effects while replicating the efficacy and safety experience of eugonadal men of similar age. Androgen replacement therapy is unlikely to prolong life because androgen deficiency, whether due to castration or biological disorder, has minimal effect in shortening life expectancy .
As an alternative, pharmacologic androgen therapy uses androgens without restriction on androgen type or dose but aims to produce androgen effects on muscle, bone, brain, or other tissues. In such pharmacological treatment, regardless of androgen status, an androgen is used therapeutically to exploit the anabolic or other effects of androgens on muscle, bone, and other tissues as hormonal drugs in various non-reproductive disorders. Such pharmacological androgen therapy is neither constrained to using the natural androgen, testosterone, nor it is limited to physiological replacement doses or their equivalent. Rather, it is judged on its efficacy, safety, and relative cost- effectiveness for that specific indication just as any other hormonal or xenobiotic non-hormonal therapeutic drug.
Many older uses of pharmacologic androgen therapy are now considered second-line therapies as more specific treatments are developed. For example, erythropoietin has largely supplanted androgen therapy for anemia due to marrow or renal failure and improved first-line drug treatments for endometriosis, osteoporosis and advanced breast cancer have similarly relegated androgen therapy to a last resort while newer mechanism-based agents in development for hereditary angioedema may displace 17a-alkylated androgens. Nevertheless, in many clinical situations, pharmacological androgen therapy remains a cost-effective option with a long-established efficacy and safety profile.
Androgen Replacement Therapy
The sole unequivocal clinical indication for testosterone treatment is in replacement therapy for androgen deficient men suffering from pathological
19 –
-disorders of their reproductive system (hypothalamus, pituitary, testis) that prevent the testes producing sufficient testosterone supply to meet the body’s usual needs. These disorders can, and often do, lead to persistent testosterone deficiency either due to disorders of the testis, where damaged Leydig cells cannot produce sufficient testosterone, or disorders of the hypothalamus and/or pituitary, where impaired pituitary luteinizing hormone (LH) secretion reduces the sole driving force to testosterone production by Leydig cells.
This treatment uses only the natural androgen, testosterone, aimed at restoring a physiologic pattern of androgen exposure using a dose limited to that which maintains blood testosterone levels within the eugonadal range.. This requires restricting replacement therapy to the major natural androgen, testosterone, which aims to not only replicate physiological circulating testosterone levels but also to provide testosterone’s two bioactive metabolites, DHT and estradiol, so that all 3 bioactive sex steroids are available to androgen target tissues.
Taking in considerations that Synthetic androgens are unsuitable because they are incapable of metabolism to the more potent 5α reduced metabolites or aromatized to estrogens.
Although life expectancy is not reduced by castration as an adult or only minimally (~2 years) shortened by life-long androgen deficiency, the hormonal deficit causes preventable morbidity and a suboptimal quality of life . Due to its variable and often subtle clinical features, androgen deficiency remains significantly underdiagnosed, thus denying sufferers simple and effective medical treatment
»Side effects
21 –
Ø When androgens are used in women, especially in high doses, male-like changes may occur, such as :
-hoarseness or deepening of the voice
-unnatural hair growth or unusual hair loss
Most of these changes will go away if the medicine is stopped as soon as the changes are noticed. However, some changes, such as voice changes or enlarged clitoris, may not go away.
Ø When androgens are used in high doses in males, they interfere with the
production of sperm. This effect is usually temporary and only happens
during the time you are taking the medicine.
Ø Although not all of these side effects may occur
a medicine may cause some unwanted effects such as :
More common
FOR FEMALES ONLY
• Acne or oily skin
• decreased breast size
• irregular menstrual cycles
FOR MALES ONLY
• hoarseness or deepening of voice
• increase in size of female genitals
• increase in unnatural hair growth or male
pattern baldness
• Blistering of skin under patch
• breast soreness or enlargement
• frequent or continuing erection of penis lasting up to 4 hours or painful penile
erections lasting longer than 4 hours
-FOR FEMALES WITH BREAST CANCER OR BEDRIDDEN MALES OR FEMALES— IN ADDITION TO THE SIDE EFFECTS LISTED ABOVE
• Confusion or mental depression
• constipation
• increased thirst
• increased urge to urinate or polyuria
FOR MALES ONLY
• frequent urge to urinate
• itching or redness of skin under patch
FOR PREPUBERTAL BOYS ONLY
• Acne
• early growth of pubic hair
Less common
FOR MALES OR FEMALES
• Dizziness
• frequent or continuing headache
• lack or loss of strength
• nausea
• overall body flushing, redness, or itching of skin
• rapidly changing moods,
• yellow skin or eyes (occurring with fluoxymesterone or methyltestosterone)
22 –
• enlargement of penis
• frequent or continuing erections
• • • •
• • • •
burning sensation or hardening or thickening of skin under patch
continuing pain at site of implants
itching, skin redness, or rash under patch, severe (less likely with nonscrotal patch) vomiting of blood or material that looks like coffee grounds
chills
difficulty in urinating
Black, tarry stools pain in scrotum or
groin
• swelling of feet or lower legs • unusual bleeding
• unusual tiredness
Contraindications
23 –
Ø Allergies
Some patients may develop unusual or allergic reaction to medicines in this group or
any other medicines.
Ø Pediatric
Androgens may cause children to stop growing. In addition, androgens may make male children develop too fast sexually and may cause male-like changes in female children
Ø Geriatric
When older male patients are treated with androgens, they may have an increased risk of enlarged prostate (a male gland) or their existing prostate cancer may get worse. For these reasons, a prostate examination and a blood test to check for prostate cancer is often done before androgens are prescribed for men over 50 years of age. These examinations may be repeated during treatment.
Ø Pregnancy
Androgens are not recommended during pregnancy. When given to pregnant women, the medicine has caused male features to develop in female babies.
Ø Breastfeeding
Use is not recommended in nursing mothers, since androgens may pass into the breast milk and may cause unwanted effects in the nursing baby, such as premature (too early) sexual development in males and development of male features in female babies.
Ø Drug Interactions
Using medicines in this class with any of the following medicines is not recommended. the doctor may decide not to treat patient with a medication in this class or change some of the other medicines that
• Phenprocoumon Simvastatin
• Acenocoumarol
• Anisindione
Ø Other Interactions
Certain medicines should not be used at or around the time of eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur.
• Atorvastatin he takes. • Bupropion
• Dicumarol
Ø Other Medical Problems
-The presence of other medical problems may affect the use of medicines in this class, especially:
• Breast cancer (in males) or Prostate cancer
Androgens can cause growth of these tumors.
• Breast cancer (in females)
Androgens may cause high calcium levels in the blood to become worse.
• Diabetes mellitus (sugar diabetes)
Androgens can increase or decrease blood sugar levels. Careful monitoring of blood glucose should be done.
• Edema (swelling of face, hands, feet, or lower legs) or Kidney disease or Liver disease
These conditions can be worsened by the fluid retention, that can be caused by androgens. Also, liver disease can prevent the body from removing the medicine from the bloodstream as fast as it normally would. This could increase the chance of side effects occurring
• Enlarged prostate
Androgens can cause further enlargement of the prostate.
• Heart or blood vessel disease
Androgens can make these conditions worse because androgens may increase blood cholesterol levels. Also, androgens can cause fluid retention , which also can worsen heart or blood vessel disease.
24 –
Anabolic steroidsAnabolic steroids are synthetic, or human- made, variations of the male sex hormone testosterone. The proper term for these compounds is anabolic-androgenic steroids. “Anabolic” refers to muscle building, and “androgenic” refers to increased male sex characteristics. Some common names for anabolic steroids are Gear, Juice, Roids, and Stackers.
»
25 –
Health care providers can prescribe steroids to treat hormonal issues, such as delayed puberty. Steroids can also treat diseases that cause muscle loss, such as cancer and AIDS. But some athletes and bodybuilders misuse these drugs in an attempt to boost performance or improve their physical appearance.
The majority of people who misuse steroids are male weightlifters in their 20s or 30s. Anabolic steroid misuse is much less common in women. It is difficult to measure steroid misuse in the United States because many national surveys do not measure it. However, use among teens is generally minimal. The 2016 NIDA-funded Monitoring the Future study has shown that past-year misuse of steroids has declined among 8th and 10th graders in recent years, while holding steady for 12th graders.
Ø anabolic steroids misuse
People who misuse anabolic steroids usually take them orally, inject them into muscles, or apply them to the skin as a gel or cream. These doses may be 10 to 100 times higher than doses prescribed to treat medical conditions. Commons patterns for misusing steroids include:
• cycling—taking multiple doses for a period of time, stopping for a time, and
then restarting
• stacking—combining two or more different steroids and mixing oral and/or
injectable types
• pyramiding—slowly increasing the dose or frequency of steroid misuse,
reaching a peak amount, and then gradually tapering off to zero
• plateauing—alternating, overlapping, or substituting with another steroid to
-avoid developing a tolerance
There is no scientific evidence that any of these practices reduce the harmful medical consequences of these drugs.
Ø Effect of anabolic steroids on the brain
Anabolic steroids work differently from other drugs of abuse; they do not have the same short-term effects on the brain. The most important difference is that steroids do not directly activate the reward system to cause a “high”; they also do not trigger rapid increases in the brain chemical dopamine, which reinforces most other types of drug taking behavior. Misuse of anabolic steroids might lead to negative mental effects, such as:
• paranoid (extreme, unreasonable) jealousy
• extreme irritability and aggression (“roid rage”) • delusions—false beliefs or ideas
• impaired judgment
• mania
26 –
-- Aside from mental effects, steroid use commonly causes severe acne.
- It also causes the body to swell, especially in the hands and feet. Long-Term Effects
Anabolic steroid misuse might lead to serious, even permanent, health problems such as:
• kidney problems or failure
• liver damage and tumors
• enlarged heart, high blood pressure, and changes in blood cholesterol, all
of which increase the risk of stroke and heart attack, even in young
people
• increased risk of blood clots
Several other effects are gender- and age-specific: • In men:
shrinking testicles
decreased sperm count
baldness
development of breasts increased risk for prostate cancer
• In women:
growth of facial hair or excess body hair decreased breast size
male-pattern baldness
changes in or stop in the menstrual cycle enlarged clitoris
deepened voice
• In teens:
stunted growth (when high hormone levels from steroids signal to the
body to stop bone growth too early)
stunted height (if teens use steroids before their growth spurt)
Some of these physical changes, such as shrinking sex organs in men, can add to mental side effects such as mood disorders.
Ø Other health effects of anabolic steroids
Anabolic Steroids and Infectious Diseases - People who inject steroids increase their risk of contracting or transmitting HIV/AIDS or hepatitis.
Ø Anabolic steroids and addiction
27 – –
Even though anabolic steroids do not cause the same high as other drugs, they can lead to a substance use disorder. A substance use disorder occurs when a person continues to misuse steroids, even though there are serious consequences for doing so. The most severe form of a substance use disorder is addiction. People might continue to misuse steroids despite physical problems, high costs to buy the drugs, and negative effects on their relationships. These behaviors reflect steroids’ addictive potential. Research has further found that some steroid users turn to other drugs, such as opioids, to reduce sleep problems and irritability caused by steroids.
People who misuse steroids might experience withdrawal symptoms when they stop use, including:
• fatigue
• restlessness
• loss of appetite • sleep problems
• decreased sex drive
• steroid cravings
• depression: One of the more serious withdrawal symptoms, which can
sometimes lead to suicide attempts
28 –
Student name:
Antonuoes Gamal Abdo Astaphanos Elsayed Eid Elsayed Omar Anti-androgens
Ø The chemistry:
»
29 –
Antiandrogens, also known as androgen antagonists or testosterone blockers, are a class that prevent androgens like testosterone and dihydrotestosterone (DHT) from mediating their biological effects in the body. They act by blocking the androgen
receptor (AR) and/or inhibiting or suppressing androgen production.
Antiandrogens can be divided into several different types based on chemical structure,
including:
- Steroidal (
) Peptides (
Ø Mechanism of action:
• Inhibitors of Androgen Biosynthesis:
Ketoconazole (Nizoral) is a broad-spectrum antifungal agent that in very high doses inhibits several steps in the biosynthesis of both adrenal and gonadal steroids. While the normal antifungal dose is 200 mg/day, testosterone biosynthesis in both the adrenal and testis is completely abolished by doses of 800 to 1,600 mg/day. This drug
like cyproterone acetate, spironolactone, estradiol, abiraterone acetate,
and finasteride
Non-steroidal (like bicalutamide, elagolix, diethylstilbestrol, aminoglutethimide,
and ketoconazole)
GnRH analogues like leuprorelin and cetrorelix.)
-is used most commonly for large virilizing adrenal tumors that cannot be surgically removed.
• Androgen Receptor Antagonists
Spironolactone (Aldactone) is a compound originally developed as a mineralocorticoid antagonist and is used as a diuretic and antihypertensive agent .However, at high doses spironolactone binds to the androgen receptor. In clinical practice it is a weak androgen antagonist used to treat hirsutism in women by blocking testosterone binding to androgen receptors in hair follicles. Use of spironolactone in women for the treatment of hirsutism or male pattern baldness can result in elevated serum potassium levels; these levels should be checked within 1 month of starting the medication.
Flutamide (Eulexin) is a nonsteroidal androgen receptor antagonist that inhibits androgen binding to its nuclear receptor. It is effective in inducing prostatic regression and is approved for the treatment of prostatic carcinoma. For maximum clinical effectiveness it has to be used in combination with a GnRH antagonist (e.g., leuprolide acetate) that inhibits androgen production. Flutamide may eventually be used for the treatment of hirsutism and male pattern baldness in women if a topical preparation is developed.
Cyproterone acetate is a progestational antiandrogen that blocks androgen receptor binding and suppresses androgen-sensitive tissues. It is available in a topical form in Europe for the treatment of hirsutism.
• 5-Reductase Inhibitors
Finasteride (Proscar) is a 5-reductase inhibitor that blocks the conversion of testosterone to DHT in target tissues. Since DHT is the major intracellular androgen in the prostate, finasteride is effective in suppressing DHT stimulation of prostatic growth and secretory function without markedly affecting libido. It is approved for the treatment of benign prostatic hyperplasia.Although there is usually some regression in the size of the prostate gland following administration of finasteride, clinical response may take 6 to 12 months. If the obstructive symptoms are severe, there is often not enough time to allow this compound to work. The principal adverse effects of finasteride are impotence, decreased libido, and decreased volume of ejaculate. The compound is generally well tolerated in men
• Gonadotropin-Releasing Hormone
Analogues GnRH analogues can induce chemical castration by suppressing the pulsatile release of LH and FSH, hence inhibiting testicular steroidogenesis. Administration of these compounds reduces circulating testosterone levels. These compounds are inhaled, injected subcutaneously, or implanted subcutaneously. They are used in males in the treatment of precocious puberty and carcinoma of the prostate.
30 –
Ø Medical uses:For men:
• Prostate cancer:
31 –
Androgens like testosterone and particularly DHT are importantly involved in the development and progression of prostate cancer They act as growth factors in
the prostate gland, stimulating cell division and tissue growth In accordance, therapeutic modalities that reduce androgen signaling in the prostate gland, referred to collectively as androgen deprivation therapy, are able to significantly slow the course of prostate cancer and extend life in men with the disease.
The most common methods of androgen deprivation therapy currently employed to treat prostate cancer are castration (with a GnRH modulator or orchiectomy), nonsteroidal antiandrogens, and the androgen synthesis inhibitor abiraterone acetate. Castration may be used alone or in combination with one of the other two treatments. When castration is combined with a nonsteroidal antiandrogen
like bicalutamide, this strategy is referred to as combined androgen blockade (also known as complete or maximal androgen blockade). Enzalutamide, apalutamide, and abiraterone acetate are specifically approved for use in combination with castration to treat castration-resistant prostate cancer.
In addition to active treatment of prostate cancer, antiandrogens are effective
as prophylaxis (preventatives) in reducing the risk of ever developing prostate cancer.
• Enlarged prostate
The 5α-reductase inhibitors finasteride and dutasteride are used to treat benign prostatic hyperplasia, a condition in which the prostate becomes enlarged and this results in urinary obstruction and discomfort. They are effective because androgens act as growth factors in the prostate gland. The antiandrogens chlormadinone
acetate and oxendolone and the functional
antiandrogens allylestrenol and gestonorone caproate are also approved in some countries for the treatment of benign prostatic hyperplasia
• Scalp hair loss
5α-Reductase inhibitors like finasteride, dutasteride, and alfatradiol and
the topical nonsteroidal AR antagonist topilutamide (fluridil) are approved for the treatment of pattern hair loss, also known as scalp hair loss or baldness This condition is generally caused by androgens, so antiandrogens can slow or halt its
progression Systemic antiandrogens besides 5α-reductase inhibitors are not generally used to treat scalp hair loss in males due to risks like feminization (e.g., gynecomastia) and sexual dysfunction However, they have been assessed and reported to be effective for this indication
-32 –
• Acne
Antiandrogens are generally not used to treat acne in males due to their high risk of feminization (e.g., gynecomastia) and sexual dysfunction. However, they have been studied for acne in males and found to be effective. Clascoterone, a topical antiandrogen, is effective for acne in males and may become approved for this indication in the future.
• Sexual deviance
Androgens increase sex drive, and for this reason, antiandrogens are able to reduce sex drive in men In accordance, antiandrogens are used in the treatment of conditions of sexual deviance such as hypersexuality (excessively high sex drive)
and paraphilias (atypical and sometimes societally unacceptable sexual interests)
like pedophilia (sexual attraction to children). They have been used to decrease sex drive in sex offenders so as to reduce the likelihood of recidivism (repeat offenses). Antiandrogens used for these indications include cyproterone
acetate, medroxyprogesterone acetate, and GnRH modulators
• Early puberty
Antiandrogens are used to treat precocious puberty in boys They work by opposing the effects of androgens and delaying the development of secondary sexual characteristics and onset of changes in sex drive and function until a more appropriate age. Antiandrogens that have been used for this purpose include cyproterone
acetate, medroxyprogesterone acetate, GnRH
modulators, spironolactone, bicalutamide, and ketoconazole. Spironolactone and bicalutamide require combination with an aromatase inhibitor to prevent the effects of unopposed estrogens, while the others can be used alone
For Women and girls:
Skin and hair conditions
Antiandrogens are used in the treatment of androgen-dependent skin and hair conditions including acne, seborrhea, hidradenitis suppurativa, hirsutism, and pattern hair loss in women. All of these conditions are dependent on androgens, and for this reason, antiandrogens are effective in treating them. The most commonly used antiandrogens for these indications are cyproterone acetate and spironolactone. Flutamide has also been studied extensively for such uses, but has fallen out of favor due to its association with hepatotoxicity. Bicalutamide, which has a relatively minimal risk of hepatotoxicity, has been evaluated for the treatment of hirsutism and found effective similarly to flutamide and may be used instead of it. In addition to AR antagonists, oral contraceptives containing ethinylestradiol are effective in treating these conditions, and may be combined with AR antagonists.
High androgen levels
Hyperandrogenism is a condition in women in which androgen levels are excessively and abnormally high. It is commonly seen in women with PCOS, and also occurs in
-women with intersex conditions like congenital adrenal hyperplasia. Hyperandrogenism is associated with virilization – that is, the development of masculine secondary sexual characteristics like male-pattern facial and body hair growth (or hirsutism), voice deepening, increased muscle mass and strength, and broadening of the shoulders, among others. Androgen-dependent skin and hair conditions like acne and pattern hair loss may also occur in hyperandrogenism, and menstrual disturbances, like amenorrhea, are commonly seen. Although antiandrogens do not treat the underlying cause of hyperandrogenism (e.g., PCOS), they are able to prevent and reverse its manifestation and effects. As with androgen-dependent skin and hair conditions, the most commonly used antiandrogens in the treatment of hyperandrogenism in women are cyproterone acetate and spironolactone. Other antiandrogens, like bicalutamide, may be used alternatively.
Transgender hormone therapy
33 –
Antiandrogens are used to prevent or reverse masculinization and to facilitate feminization in transgender women who are undergoing hormone therapy and who have not undergone sex reassignment surgery or orchiectomy. Besides estrogens, the main antiandrogens that have been used for this purpose are cyproterone acetate, spironolactone, and GnRH modulators.Nonsteroidal antiandrogens like bicalutamide are also used for this indication.In addition to use in transgender women, antiandrogens, mainly GnRH modulators, are used as puberty blockers to prevent puberty in transgender girls until they are older and ready to begin hormone therapy.
The largest organ covering the whole body
Functions of skin
Barrier against: -U.V rays (by melanin)
-Infection, trauma, dehydration (by keratin) 2-Receives sensations (by receptors)
3-Regulate body temperature (sweat glands)
1-Protection:
4-Excrete
5-Synthesis of vitamin D
6-Medico-legal importance (Finger prints) 7-Diagnosis of some diseases
(anemia, measles, chicken pox, jaundice).
waste products (sweat glands)
Types of skin
■1-Thick skin ■2-Thin skin
Thick Skin
■ Site:
-Palm of hands
-Sole of feet
-Tips of fingers & toes
Structure of Skin
■ ■ ■
Epidermis Dermis Skin
Appendages:
A-Hairs B-Glands C-Nails
I- Epidermis
■ keratinized stratified squamous epith.:
A-Keratinocytes:
85% of cells &
Form keratin B-Non-keratinocytes:
1-Melanocytes 2-Merkel’s cells 3-Langerhans cells
A- Keratinocytes
■5 Layers:
■1-Basal [Germinal] cell layer ■2-Spinous [Prickle] cell layer ■3-Granular layer
■4-Clear layer
■5-Horny layer
1-Basal [Germinal] cell layer
■ L.M:
1 layer of columnar cells
■
■ Resting on clear & wavy B.M
■ Basal oval nuclei [++ mitotic figures for renewal]
■ Renewal occurs every 2-4 weeks mostly at night
■ Basophilic cytoplasm
1-Basal [Germinal] cell layer
■ E.M:
■ Cells joined together by desmosomes
& to B.M by hemi-desmosomes ■ Rich in ribosomes & polysomes N.B: Melanocytes + Merkel’s cells
are present in this layer
2-Spinous [Prickle] cell layer
■ L.M:
■ 4-9 layers of polyhderal cells
■ Central rounded nuclei
■ Less basophilic cytoplasm
■ Cells have spine- like processes [Indicate sites of desmosomes as cells shrink during preparation]
2-Spinous [Prickle] cell layer
2-Spinous [Prickle] cell layer
■ E.M:
■ Cells joined by desmosomes have interdigitating
cell membranes
■ Superficial cells contain membrane
bound (coated) lamellar granules N.B: Langerhans cells are present
in this layer
■Basal layer together + Spinous layer are called Malpighian layer
3-Granular layer
■ L.M:
■ 2-4 layers of spindle- shaped cells ■ Flat nuclei
■ Basophilic granules
■ E.M: 2 types of granules:
a) Coated lamellar granules b) Keratohyaline granules
a) Coated lamellar granules
■ Oval or rod-shaped
■ Covered by membrane ■ Contain lamellar discs
[Lipid bilayers]
■ Discharge their content to
intercellular space → Lipid sheets
→ Act as cement & barrier against bacteria
b) Keratohyaline granules:
■ Large
■ Not covered by membrane ■ Form matrix →
Bind tonofilaments → Form bundles
4-Clear layer
■ L.M:
■ 1 layer of flat cells ■ No Nuclei
■ E.M:
■ No Nucleus or organelles
■ Cells joined by remnants of desmosomes
■ Contain packed filaments of eleidin [immature keratin] embedded in matrix [Formed by keratohyaline granules]
5-Horny layer
■ L.M:
■ Many acidophilic layers or scales
of keratinized dead cells
■ E.M:
■ Dead cells
■ No nuclei or organelles
■ Joined by remnants of desmosomes
■ Filled with mature keratin filaments embedded in matrix
B-Non-Keratinocytes
1] Melanocytes
■ Origin: Ectodermal ■ L.M:
■ Pale round nuclei
■ Long processes
to transport melanin to adjacent cells
■ Give Dopa +ve reaction [Dihydroxyphenylalanine]
Application of DOPA to skin → Dark color due to formation of melanin by tyrosinaze enzyme
1] Melanocytes
■ E.M:
■ Euchromatic nucleus ■ Prominent nucleolus ■ No desmosomes
between them & keratinocytes
■ Joined to B.M by hemi-desmsosmes ■ Characters of ptn. forming cells:
[+++ Mitochondria, rER & G.A]
1] Melanocytes
■ Function:
■ 1-Form tyrosinase enz.
→ Form melanin →
Gives skin colour
■ 2-Melanin granules protect DNA from UVRs
1] Melanocytes
2- Merckel’s cells:
■ Origin: Ectodermal ■ L.M:
■ Modified basal cells
[But slightly larger]
■ Naked sensory nerve fibres end in disc like expansion under these cells
2- Merckel’s cells:
■ E.M:
■ Attached to adjacent cells
by desmosomes
■ Cytoplasm contains electron-dense granules
[So, it belongs to APUD cells]
■ Functions:
■ 1-Mechanoreceptor for (touch & pressure) ■ 2-Paracrine regulation of epidermal cells
3-Langerhans cells
■ Origin: Mesodermal
■ L.M:
■ Branched cells between
cells of spinous layer ■ Dark nucleus
■ Pale cytoplasm
3-Langerhans cells
■ E.M:
■ 1ry & 2ry lysosomes ■ Well developed G.A ■ Birbeck’s granules:
[Tennis-raquet-shaped, contain hydrolytic enzs.] ■ No desmosomes
■ No junctions with keratinocytes
■ Function:
■ 1-Phagocytic cells of skin
■ 2-Antigen presenting cells [present antigens to T- lymphocytes]
II- Dermis
■ Connective tissue under epidermis
Dermis is formed of 2 layers
■Papillary layer ■Reticular layer
Papillary layer
Reticular layer
-Thinner & superficial -Loose C.T
-More cellular
-More vascular -Receptors: •Meissner’s corpuscles
-Thicker & deeper -Dense fibrous C.T -Less cellular -Less vascular -Receptors:
•Pacinin corpuscles •Krause end bulb+ •Ruffini end organ
Thick skin
Thin skin
Sties:
-Palms & soles
-Tips of fingers & toes
The rest of body
Epidermis
Thick
Thicker Malpighian layer Thicker granular (2-4Ls) Clear L present
Thick Horny layer
Thinner Thinner Thinner (1L) Absent Thinner
Dermal papillae
Regular, Numerous & High
Few Irregular
Appendages
No hair follicles
No arrector pili muscle No Sebaceous glands Numerous sweat glands
Present Present Present
Less numerous
Skin Appendages
■ ■ ■
A-Hairs B-Glands C-Nails
Thin hairy skin
A-Hairs
■ Def:
keratinized epithelial thread inserted into epidermal sheath
Structure:
1-Shaft:
Projects above skin surface
2-Root:
Embedded in skin
3-Hair bulb:
Terminal dilatation
Both shaft & root are formed of:■Medulla: Soft keratin
■Cortex: Hard keratin [contain melanin] ■Cuticle: Hard keratin
■3-Hair bulb [Terminal dilatation]
-Invaginated by vascular C.T
→ Hair papilla
-Contains:
1-Melanocytes
2-Matrix cells for growth of hair
Hair Follicle
■ Downgrowth of epidermis around root of hair ■ Formed of 3 sheaths:
1-Inner root sheath
2-Outer root sheath
3-Connective tissue sheath
1-Inner root sheath
3 layers:
• Cuticle:
Scales rich in soft keratin
• Huxley’s layer:
2-3 layers
• Henle’s layer: 1 layer
■2-Outer root sheath
■ Downward continuation of epidermis
■ At bottom → Basal layer only
■ 3-Connective tissue sheath → C.T dermis
Colour of hair
■ Caused by melanin pigment in cortex
■ Produced by melanocytes in hair matrix
■ Grey hair: In old age melanocytes fail to produce tyrosinase
■ Yellow hair: Due to pheomelanin (yellow)
■ Baldness: Hair loss due to genetic factors & sex hormones [Mainly in males]
Arrector Pili Muscle
■ Smooth muscle
■ Origin:
Papillary layer of dermis ■ Insertion:
Sheath
■ Its contraction: (By fear or cold) → Erection of
hair & depression of skin → Goose skin
B- Glands of Skin
■ 1-Sweat Glands
■ 2-Sebaceous Glands
?
a- Eccrine sweat glands
b- Apocrine seat glands
Type
Simple coiled tubular gland
Mode of secretion
Merocrine
Apocrine
Site
-All over the body -More in thick skin
-Thin skin of axilla -Pubic & perineal areas
Acini
-Lined with 2 types of cuboidal cells -Surrounded by myoepith. cells
1-Large pale [clear] cells -Broad base & narrow apex -Pale cytoplasm (glycogen)
2-Small dark cells
-Narrow base & broad apex -Dark granular cyt. (glycoptn)
a- Eccrine sweat glands
b- Apocrine seat glands
Ducts
Spiral course in epidermis & open into
Epidermis
Hair follicle
Lined with 2 layers of cubical cells
Function
→ Clear watery sweat [H2O + NaCl + urea +
ammonia]
→ Odourless sweat → by bacteria → Offensive
odour
(Start function at puberty)
2-Sebaceous gland
■ Type:
Simple or simple branched alveolar gland
■ Mode of secretion:
Holocrine
■ Site:
Associated with hair follicles
2-Sebaceous gland
■ Acini: Lined with: 1-Basal flat stem cells
to replace
2-Central polyhedral cells
with central nuclei
& vacuolated cytoplasm (fat)
2-Sebaceous gland
■ Ducts:
-Short
-Open into upper 1/3 of
hair follicle
-Lined with stratified
squamous epith.
■ Function:
Secrete sebum (oily) to prevent cracking of skin
Sebaceous gland
C-Nails
■ Def:
Plates of keratinized epith. cells
on dorsum of distal phalanx
■ Formed of:
Nail plate + Free edge + Root
(in nail groove, covered by nail fold)
■ Proximal nail fold:
Skin fold which covers the root
■ Lateral nail fold:
2 skin folds that cover lateral sides ■ Nail bed:
■ Area under nail plate: 1-Epidermal cells:
Thin malpighian layer
2-Dermis:
Highly vascular with
no papillae
■ Nail Matrix:
Malpighian cells
lining the nail groove from which the nail grows
■ Lunula: Crescent-shaped white area at the base of nail plate
Quiz 1- As regards entamoeba histolytica life cycle , ingestion of binucleate cyst causes :- a. Amoebiasis
b. Amoebic dysentery c. All of the above
d. None of the above - Flask shaped ulcer in the rectosigmoid colon may result in :-
a. Amoeboma
b. Post-dysenteric ulcerative colitis
c. All of the above
d. None of the above - Blood
a. Leukocytosis
picture of a patient suffers from amoebic liver abscess shows :-
b. Cyst
c. Trophozoite d. Anemia - Presence of massive exudate in stool sample indicates infection with :-
a. Entamoeba histolytica
b. Entamoeba dispar
c. Bacteria
d. Both b and c - As regards amoebiasis , positive serologic titres can be detected in :-
a. None-invasive intestinal amoebiasis
b. Hepatic amoebic abscess
c. Invasive intestinal amoebiasis
d. Both b and c - As regards acanthamoeba spp. Infection , skin scraping shows :-
a. b. c. d. - In case
a. b. c. d.
Trophozoite Cyst
Biflagellate form Both a and b
of amoebic ulcer , rectal scraping shows :-
Leukocytosis Binucleate cyst Trophozoite Quadrinucleate cyst - As regards Entamoeba histolytica , ingestion of quadrinucleate cyst causes :-
a. Amoebiasis
b. Amoebic dysentery
c. All of the above
d. None of the above - Presence of scanty exudate in stool sample indicates infection with :-
a. Entamoeba histolytica
b. Entamoeba dispar
c. Bacteria
d. Both b and c - Acanthamoeba can be a problem for the following people except :-
a. Who swim in super chlorinated water
b. Who wear contact lenses
c. Who swim in stagnant warm fresh water
d. Both b and c - Which of the following protozoa is opportunistic ?
a. Acanthamoeba spp.
b. Naegleria fowleri
c. Entamoeba histolytica - What do you suspect to see in CSF of patient complaining of chronic granulomatous amoebic encephalitis ?
a. Trophozoite b. Cyst c.
d. 13. Flask a. b. c. d.
Biflagellate form
Both a and b
shaped ulcer in recto-sigmoid colon may result from infection by :-
Entamoeba histolytica
Bacteria Entamoeba dispar a and b - entamoeba histolytica probably spread from the intestine to liver via :-
a. portal circulation
b. peritoneal cavity
c. all of the above
d. none of the above - presence of charcot –leyden crystals in stool sample indicates infection with :-
a. entamoeba histolytica
b. entamoeba hartmanii
c. bacteria
d. both b and c - extra- intestinal amoebiasis , can be treated with :-
a. metronidazole
b. chloroquine
c. diloxanide furoate
d. all of the above - as regards acanthamoeba spp. Infection , skin scraping shows :-
a. trophozoite
b. cyst
c. biflagellate form
d. a and b - as regards naegleria fowleri infection microscopic examination of CSF shows :-
a. trophozoite
b. cyst
c. biflagellate form
d. all of the above - which of the following parasite is highly endemic in Egypt :-
a. entamoeba coli
b. entamoeba histolytica
c. acanthamoeba spp.
d. All of the above - The following parasites cause dysentery except :-
a. Entamoeba histolytica
b. Entamoeba coli
c. Balantidium coli - The following intestinal amoeba trophozoites have sluggish motility except :-
a. Iodamoeba butschlii
b. Dientamoeba fragilis
c. Entamoeba histolytica
d. Endolimax nana - Which of the following parasite is transmitted to man through autoinfection?
a. Naegleria fowleri
b. Balantidium coli
c. Acanthamoeba spp. - Which of the following parasitic diseases can be prevented by examination and treatment of food handlers?
a. Amoebiasis
b. Balantidiasis
c. All of the above
d. None of the above - As regards balantidiasis all of the following are true except :-
a. Trophozoite secrete proteolytic enzyme
b. Causes extra-intestinal lesions
c. Intestinal perforation may occur
d. Drug of choice metronidazole - In sigmoidoscopy of flask shaped ulcer of entamoeba histolytica , stage seen is :- a. Trophozoites
b. Cyst
c. Biflagellate from d. None of the above - In sigmoidoscopy of flask shaped ulcer of entamoeba histolytica , trophozoite seen in :-
a. Edge of ulcer
b. Base of ulcer
c. A and b
d. None of the above - Oxytetracyclin used to treat :-
a. Entamoeba histolytica
b. Naegleria fowleri
c. Balantidium coli - Amphotericin B used to treat :-
a. Entamoeba histolytica
b. Naegleria fowleri
c. Balantidium coli - Which of the following protozoa have reservoir hosts :-
a. Entamoeba histolytica
b. Naegleria fowleri
c. Balantidium coli - Which of the following parasite has 3 morphological stages
a. Naegleria fowleri
b. Balantidium coli
c. Acanthamoeba spp. - Confirmatory test in naegleria shows :-
a. Cyst
b. Trophozoite
c. Biflagellate form d. None of the above - As regards entamoeba histolytica all of the following are true except :-
a. Trophozoite secrete proteolytic enzymes
b. Cause extra-intestinal lesions
c. Cause duodenitis
d. Infective stage is cyst - Microscopic examination of aspirate from amoebic liver abscess reveals :- a. Trophozoite
b. Cyst
c. A and b
d. None of the above - Anchovy sauce appearance of liver abscess occur in case of :-
a. Entamoeba histolytica
b. Balantidium coli
c. Naegleria fowleri - Only amoeba has additional morphological form ( biflagellate form) is :-
a. Entamoeba histolytica
b. Balantidium coli
c. Naegleria fowleri
36- Trophozoite form of amoeba are most likely to be found in :-
a- Semi-formed stool
b- Hard stool
c- Diarrheal stool
d- All of the above
37- The amoeba having a flagellate form is :-
a- Trichomonas vaginalis
b- Naegleria fowleri
c- Acanthamoeba
d- All of the above
38- All these are pathogenic protozoa except :- a- Entamoeba histolytica
b- Entamoeba coli ( OR E. hartmanii , E.dispar )
c- Balantidium coli
d- Giardia lamblia
39- Which of the following cause primary amoebic encephalitis ( PAM) :-
a- Entamoeba histolytica
b- Dientamoeba fragilis
c- Naegleria fowleri
d- Balantidium coli
40- The amoebic liver abscess :-
a- Associated with eosinophilia
b- Associated with lymphadenopathy
c- Associated with portal HTN
d- Should be aspirated , reveals anchovy sauce appearance
41- Charcot leyden crystals appear in stool in infection with :-
a- Entamoeba histolytica
b- Entamoeba coli
c- Bacillary dysentery
d- Trichomonas vaginalis
42- Metronidazole is not indicated in treatment of :-
a- Trichomonas vaginalis
b- Entamoeba histolytica
c- Balantidium coli
d- Acanthamoeba
43- A flask shaped ulcer develop in :-
a- Entamoeba histolytica
b- Balantidium coli
c- Giardia lamblia
d- A,b
44- The patient pass stool with mucous tinged with blood in :-
a- Entamoeba histolytica infection
b- Trichomonas vaginalis infection
c- Giardia lamblia infection
d- Trichomonas vaginalis infection
45- Stool in bacillary dysentery is :-
a- Bulky & offensive
b- Alkaline
c- Acidic
d- Contain charcot leyden crystals
46- Stool in amebic dysentery is :-
a- Bulky & offensive & acidic
b- Bulky & offensive & alkaline
c- Contain bacteria
d- Contain numerous altered RBCs & pus cells
47- In invasive intestinal amoebiasis , diagnosis done by
a- Stool examination
b- Serological tests
c- Radiological tests
d- A&b
48- As regards balantidium coli , all are correct except :-
a. Infective stage is mature cyst
b. Definitive host is man
c. Has only 1 reservoir host
d. Mode of infection is ingestion Mid term - Which of the following antigens is used in montenegero test :- e. Suspension of killed promastigotes
f. Suspension of killed epimastigotes g. Suspension of killed trypomastigotes h. Suspension of killed amastigotes - To diagnose cutaneous leishmaniasis , biopsy is better taken from :-
e. Base of ulcer
f. Edge of ulcer
g. Lymph node draining the ulcer
h. Skin around the ulcer - Why does immune system not protective against trypanosomes :-
e. They have an anti-phagocytic capsule
f. They are obligate intracellular parasites
g. They continuously change their surface antigens
h. They cause lysis of T-cells - Which of the following parasites causes malabsorption syndrome :-
e. Entamoeba histolytica
f. Giardia lamblia
g. Balantidium coli
h. Leishmania donovani - Each of the following statements concerning Kala-azar is correct , except :-
e. Kala-azar caused by leishmania donovani
f. Kala-azar is transmitted by bite of sand flies
g. Kala-azar occurs primarily in north America
h. Kala-azar can be diagnosed by finding amastigotes in bone marrow - Which of the following form is detected in saliva of tsetse fly :-
e. Epimastigotes
f. Amastigote
g. Trypomastigotes h. Promastigotes - Which of the following parasitic diseases can affect the gall bladder:- e. Giardiasis
f. Trichomoniasis g. Balantidiasis
h. Leishmaniasis - As regards leishmania tropica major all of the following are true , except :-
e. Cause urban sore
f. Cause zoonotic disease
g. Present in central Asia and parts of Africa
h. Rodents are main reservoirs - Which of the following parasite invades blood and draining lymph capillaries:-
e. sarcocystis
f. plasmodium
g. polymorphic trypanosomes
h. cryptosporidium
45. which of the following parasites causes lymphadenopathy :- e. plasmodium
f. giardia lamblia
g. naegleria fowleri
h. leishmania donovani - which of the following parasites causes kerandel’s sign :-
d. polymorphic trypanosomes .
e. monomorphic trypanosomes
f. Giardia lamblia
g. Acanthamoeba - Why was plasmodium falciparum associated with CNS manifestations ?
e. Due to continuous or irregular fever
f. Due to autoimmune disease
g. Due to hyperactivation of B-lymphocytes
h. Due to adhesion phenomenon - B-thalassemia protects from infection with :-
e. Plasmodium malariae
f. Plasmodium vivax
g. Plasmodium ovale
h. Plasmodium falciparum - What is the trigger mechanism of black water fever:-
e. Lymphocytic infiltration of liver
f. Irregular doses of Quinine
g. Persistent low parasitemia
h. Presence of hypnozoites - Which of the following parasites causes depression of cellular immunity in human:-
e. Plasmodium ovale
f. Giardia lamblia
g. Leishmania donovani
h. Trichomonas vaginalis - Morula cells is detected in CSF examination in infection with :-
e. Trypanosome gambiense
f. Giardia lamblia
g. Trypanosome cruzei
h. Leishmania tropica - Stained smears from organs in Kala –azar show :-
e. Epimastigote f. promastigote g. trypomastigote h. amastigote - protozoa causing conjunctivitis include:-
e. trypanosoma gambiense
f. trypanosoma rhodesiense
g. trypanosome cruzei
h. leishmania donovani - to diagnose chronic chagas’ disease , biopsy is better taken from :-
e. lymph node
f. spleen
g. blood
h. both a and b - in early diagnosed cases of T.rhodesiense , why does serodiagnosis give false negative results :-
d. humoral antibody will be less than seen in T.gambiense
e. depression of immunity
f. Both a and b - Invasion of blood & lymphatics by T.gambiense is marked by :-
e. Fever
f. Painful sensitivity of palms to pressure
g. Both a and b - Which of the following infection can be prevented by screening of blood donors ?
d. Acute African trypanosomiais (sleeping sickness)
e. Chronic African trypanosomiais (sleeping sickness)
f. American trypanosomiais (chagas’ disease)
g. All of the above - Posterior shift of nucleus occurs in ?
e. T. cruzei
f. T. gambiense
g. T. rhodesiense
h. None of the above 1-
2-
3-
4-
5-
6-
7-
a. b. c. d.
8-
a.
b.
c.
d.
9-
a. b. c. d.
MCQs
Entamoeba histolytica trophozoites are found in: a.Duodenum of infected human.
b. Jejunum of infected human.
c. Caecum of infected human.
d. Ileum of infected human.
Infection with Entamoeba histolytica occurs through eating green salad contaminated with:
a.
b.
c.
Trophozoites of Entamoeba histolytica.
Cysts of Entamoeba histolytica.
Both trophozoites and cysts of Entamoeba histolytica.
Pathogenicity of Entamoeba histolytica depends on: a.Parasite virulence.
b. Condition of intestinal tract.
c. Host resistance.
d. All of the above.
Patients with chronic intestinal amoebiasis suffer from:
a.
b.
c.
d.
Dysentery, tenesmus with painful spasm of anal sphincter.
Recurrent attacks of dysentery alternating with constipation.
Fever, diarrhea, and tenesmus.
None of the above.
The following findings in stool suggest amoebic not bacillary dysentery infection:
a.
b. c. d.
Acidic pH and presence of Charcot Leyden Crystals.
Alkaline pH and presence of Charcot Leyden Crystals. Alkaline pH and absence of Charcot Leyden Crystals. Massive exudate with presence of many pus cells.
Microscopic examination of an aspirate from amoebic liver abscess reveals:
a.
b.
c.
d.
Haematogenous spread from keratitis lesion. Penetration from cribriform plate.
Haematogenous spread from lower respiratory tract. Haematogenous spread from liver abscess.
The trophozoite is the infective stage in:
Giardia lamblia
Trichomonas vaginalis
Entamoeba histolytica Entamoeba coli
The protozoan parasite without a cyst stage is:
Entamoeba histolyica Giardia lamblia
Entamoeba coli
Trichomonas vaginalis
Entamoeba histolytica trophozoites & cysts Entamoeba histolytica trophozoites.
Entamoeba histolyica cysts.
Entamoeba coli trophozoites & cysts. Acanthamoeba trophozoites reach the brain by:
10- Stained smears from organs in kala-azar show:
a. Epimastigote form
b. Amastigote form
c. Promastigote form d. Trypomastigote form
11- To diagnose cutaneous leishmaniasis, biopsy is better taken from:
a. base of the ulcer
b. lymph node draining the ulcer
c. edge of the ulcer
d. skin around the ulcer
12- The following arthropod transmits visceral leishmaniasis: a. Culicoides
b. Simulium
c. Chrysops
d. Phlebotomus
13- Protozoal infections that may cause fever and hepatosplenomegaly
a. Visceral leishmaniasis
b. African trypanosomiasis (sleeping sickness)
c. American trypanosomiasis (Chagas’ disease)
d. Non of the above
e. All of the above
14- Smear taken from the edge of oriental sore reveals: a. promastigote
b. amastigote
c. epimastigote
d. trypomastigote
15- Protozoa causing conjunctivitis include:
a. Trypanosoma cruzi
b. T. brucei gambiense
c. T. brucei rhodesiense
d. Leishmania donovani
16- Winterbottom’s sign is seen in:
a. b. c. d.
Cutaneous leishmaniasis Visceral leishmaniasis African trypanosomiasis
American trypanosomiasis
17- In African trypanosomiasis, the infective stage is found in:
Short stumpy metacyclic trypanosomes Saliva of Triatoma
Saliva of Glossina
Stool of Triatoma
Stool of Glossina
18- Posterior nuclear shift occurs in:
a. Trypanosoma cruzi
b. Trypanosoma gambiense
c. Trypanosoma rhodesiense
d. Trichomonas vaginalis
19- In chronic Chagas’ disease, the main lesions are in:
a. Digestive and respiratory tracts.
b. Heart and liver.
c. Heart and digestive tract.
d. Liver and spleen.
20- Megacolon associated with Chagas’ disease:
a. Is manifested by diarrhoea.
b. Occurs early in the disease.
c. Is due to oedema of the mucosa.
a. b. c. d. e.
d. Is associated with constipation. 21- In malaria, sporogony occurs in:
a. b. c. d.
Human RBCs Human liver cells Female Anopheles
Cerebral blood vessels
22- Adherence of the parasitized red cells in P. falciparum infection is the cause of:
a. black water fever
b. cerebral malaria
c. malarial recrudescence
d. malarial relapse
23- Pathogenesis of vivax malaria is mainly due to:
a. Persistence of hypnozoites in the liver.
b. Rupture of hepatocytes & release of schizont content.
c. Rupture of RBCs & liberation of pigment & parasite products.
d. Formation of gametocytes in blood stream.
24- Recrudescence in malaria is due to:
a. b. c. d.
Infection transmitted by blood transfusion. Incomplete eradication of asexual blood stages. Persistent gametocyte in RBCs.
Activation of hypnozoites.
25- Manifestations of congenital toxoplasmosis can be first seen in: a. neonatal period
b. adulthood
c. childhood
d. all of the above
26- Toxoplasmosis is fatal in AIDS patients by causing:
a. Nephrotic syndrome
b. Disseminated encephalitis
c. Megacolon & constipation
d. Megaoesophagus & dysphagia
27- Oocysts of Toxoplasma gondii is found in:
a. Brain of chronic patients
b. Tissues of infected man
c. Faeces of infected cats
d. Faeces of infected man
28- Blindness caused by Toxoplasma is due to:
a. Corneal opacity
b. Optic neuritis
c. Retinochoroiditis
d. Panophthalmitis
29- Hydrocephalus can occur in the following conditions:
a. b. c. d.
Cerebral malaria
Naegleria encephalitis Cerebral toxoplasmosis Sleeping sickness
30- Tissue cysts of Toxoplasma occur in:
a. b. c. d.
Stool of cat Stool of man
Human brain
Human blood
-31
a. b. c. d. e.
-32
a. b. c. d.
-33
a.
b.
c.
d.
-34
a. b. c. d.
-35
a.
b.
c. -36
-37
-38
The Sequelae الآثار الناتجة عن of infection with Toxoplasma depends on: immune status of infected human
age of infected human
virulence of the infecting parasite strain none of the above
all of the above
Tissue cyst of Toxoplasma is found in: Stool of cat
Infected human blood
Meat of cattle
All of the above
Microsporidia infect host cell through:
Attachment to host cell by sucking disk.
Injection of sporoplasm through polar filament.
Lysis of host cell membrane by lytic enzymes.
Phagocytosis of opsonized spore.
Microsporidiaaffects:
The human cornea
The human muscles The human intestine All of the above
Which of the following protozoa may cause dysentery?
Cryptosporidium parvum oocysts Entamoeba histolytica cyst Trichomonas vaginalis trophozoites
A patient presenting with dysentery, the patient was infected by the following method:
a. Bite of female sandfly
b. Contamination of skin abrasions by Triatoma faeces
c. Flies contaminating food by quadrinucleate cyst
A patient presenting with dysentery, If the patient was not properly treated, the following complication may occur:
a- Haemoglobinuria
b- Appendicitis
c- Nephrotic syndrome
Which of the following protozoa may cause dysentery?
a. Toxoplasma gondii tachyzoites b. Balantidiun coli trophozoite c. Giardialambliatrophozoites
39- Which of the following protozoa may cause haemolytic anaemia? a. Leishmania amastigotes
b. Gametocyte stage of P.falciparum
c. Polymorphictrypanosomes
40- A patient presenting with haemolytic anaemia , the patient was infected by the following method:
a. Bite of female Anopheles
b. Contamination by Triatoma faeces
c. Bite of sandfly
41- A patient presenting with haemolytic anaemia , Which of the following is the cause of anaemia?
a. Bonemarrowaffection
b. Destruction of RBCs
c. Decreased iron intake in food

42- Which of the following protozoa may cause aplastic anaemia? a. Leishmania amastigotes
b. Ring stage of Babesia
c. Toxoplasmagondiitrophozoites
43- Which of the following protozoa may cause hepatosplenomegaly?
a. G.lamblia trophozoite
b. Leishmania amastigotes
c. Balantidium coli cyst
44- A patient presenting with hepatosplenomegaly , Diagnosis is confirmed by the following method:
a. Detection of parasite by skin test
b. Detection of parasite in bone marrow
c. Detection of parasite in stool
45- Which of the following protozoa may cause hepatosplenomegaly? a. G.lamblia trophozoite
b. Polymorphic trypanosomes
c. B.colicyst
46- Which of the following protozoa may cause appendicitis? a. G.lamblia trophozoite
b. Balantidium coli trophozoite
c. Entamoebacolicyst
47- A patient presenting with appendicitis , The causative protozoa produces the following lesion:
a. Ulcer with sharp-cut edge & indurated margin
b. Flask-shaped ulcer
c. Nodularlesion
48- A patient presenting with appendicitis , The causative protozoa may produces the following complication: a. Spread of protozoa to liver or lungs
b. Perforation & peritonitis
c. Steatorrhoea&malabsorption
49- Myiasis is invasion of human tissues by: a- Larva of Pulex
b- Larva of Aedes
c- Larva of Sarcophaga
d- Larva of D.medinensis
50- In African trypanosomiasis, the infective stage is found in: a- Saliva of Glossina
b- Saliva of Phlebotomus c- Stool of Glossina
e- Stool of Phlebotomus
51- A patient presenting with corneal ulcer , Which of the following parasites can cause corneal ulcer?
a. E.histolytica trophozoite
b. Acanthamoeba trophozoite
c. Trypanosoma cruzi
52- A patient presenting with corneal ulcer , Which of the following represents the mode of infection by the causative protozoa?
a. ContaminationbyTriatomafaeces
b. Use of contaminated contact lens
c. Flies standing on eyes & face
53- A patient presenting with corneal ulcer , How can you confirm your diagnosis? a. Sample suspension in fresh water
b. CSF examination to detect the parasite
c. Cornealscrapingtodetecttheparasite
54- A patient presenting with swollen eye-lid , Which of the following parasites can cause swollen eye?
a. Toxoplasma gondii trophozoite b. Acanthamoeba trophozoite
c. Trypanosomacruzi
55- A patient presenting with swollen eye , Which of the following represents the mode of infection by the causative protozoa
a. Contamination by Triatoma faeces
b. Use of contaminated contact lens
c. Flies standing on eyes & face
56- A patient presenting with swollen eye , How can you confirm your diagnosis?
a. Sample suspension in fresh water
b. Blood film examination
c. Corneal scraping to detect the parasite
57- Fleas transmit the following except:
a. Epidemictyphus
b. Plague
c. Endemic typhus
d. Hymenolepis diminuta
58- Scrub typhus is transmitted by:
a- Indirect mechanical transmission.
b- Cyclopropagative transmission.
c- Cyclodevelopmental transmission. d- Trans-stadial transmission.
59- Winterbottom’s sign is seen in: a- Toxoplasmosis
b- Leishmaniasis
c- African trypanosomiasis
d- Acute Chagas’ disease
60- The following statement is NOT true for Cryptosporidiosis:
a- It is a self limited disease in immunocompetent persons. b- Bloody diarrhea is associated with infection.
c- Atrophy of intestinal villi is the cause of malabsorption. d- Both external & internal autoinfection may occur.
61- Charcot Leyden crystals appear in stool in infection with:
a. Entamoeba histolytica
b. Babesia divergens
c. Enterobius vermicularis
d. Diphyllobothrium latum
62- The human flea is the vector of the following disease
a.
b. c. d.
Plague
Epidemic relapsing fever Vagabond’s disease Trench fever
63- Female Anopheles transmits: a- Trichinosis
b- Human malaria
c- Onchocerciasis d- Chagas’ disease
64- The following arthropod transmits cutaneous leishmaniasis:
a.
b. c. d.
Phlebotomus
Tunga pentrans
Simulium Aedes aegypti
65- The following protozoa can evade the immune system by antigen variation: a- American trypanosomes
b- African trypanosomes
c- Leishmania donovani
d- Toxoplasma gondii
66- In diagnosing cutaneous leishmaniasis, biopsy is better taken from:
a.
b. c. d.
edge of the ulcer
base of the ulcer
skin around the ulcer
lymph node draining the ulcer
67- Cyclops is NOT the intermediate host in the following infection:
a. b. c. d.
a- Giardiasis
b- Cryptosporidiosis c- Cyclosporiasis
d- Isosporiasis
69- The following arthropod transmits visceral leishmaniasis: a- Triatoma
b. Tunga pentrans
c- Phlebotomus
d- Culicoides
70- Tissue cysts of Toxoplasma gondii develop in:
a- skin of the patient
b- organs of the patient
c- small intestine of the patient
d- large intestine of the patient
71- The following disease is caused by fleas: a- Trench fever
b- Epidemic typhus
c- Scrub typhus
d- Chigger’s disease
72- Ocular myiasis is caused by:
a.
b.
c.
d.
Aedes aegypti
Oestrus ovis
Culicoides
Simulium
D.latum infection D.mansoni infection D.medinensis infection
D. caninum infection
68- Autoinfection DOES NOT occur in the following parasitic infections:
73- Cutaneous nodular myiasis may occur by:
a. b. c.
Culex pipiens Tunga penetrans
Pediculus
d. Cordylobia
74- If Leishmania tropica ulcer is left without treatment the following occurs:
a.
b.
c.
d.
spreading occurs to mucus membrane
development of disfiguring scar & solid immunity
spreading occurs eroding cartilage
ulcer heals leaving no trace behind
75- Sabin Feldman dye test is used to diagnose:
a. African trypanosomiasis
b. Cryptosporidium infection
c. Toxoplasma infection
d. Plasmodium infection
76- Malaria parasites that have an affinity for old red cells include:
a. b. c. d.
Plasmodium vivax Plasmodium falciparum
Plasmodium malariae
Plasmodium ovale
77- Hyper reactive malarial splenomegaly is due to: a- Suppression of NK cells
b- Reduction of T suppressor cells
c- Reduction of B lymphocytes
d- Suppression of Macrophages
78- Cardiac lesion occurring in Chagas’ disease is due to: a- Granuloma formation
b- Immune complex deposition c- Allergic reactions
d- Autoimmune disease
79- Severe anaemia occurring in falciparum malaria is due to: a- parasite invades RBCs at all ages
b- parasite haemolyzes RBCs in a short time c- parasite induces hypersplenism
d- parasite induces knobs on RBCs surface
80- The sequelae of infection with Toxoplasma DO NOT depend on the following:
a.
b.
c.
d.
the immune status of infected human
the sex of infected human
virulence of the infecting parasite strain
the age of the infected human
81- Trophozoites of Naegleria fowleri are NOT detected in: a- wet mount of cerebrospinal fluid of patient.
b- Giemsa-stained tissue smear of patient.
c- Giemsa-stained blood film of patient.
d- cultured cerebrospinal fluid of patient.
82- The sequelae of congenital infection with Toxoplasma DO NOT depend on the following: a- the protective immunity of the pregnant mother
b- the age of the foetus at the time of infection
c- the sex of the foetus
83- Relapse occurring in P.vivax & P.ovale is due to:
a- low grade parasitaemia with lowered immunity.
b- reactivation of hypnozoites in the liver.
c- Rupture of hepatocytes & release of schizont content.
d- Formation of gametocytes in blood stream.`
84- The following is NOT an obligate intracellular parasite: a- Giardia lamblia
b- Leishmania tropica c- Plasmodium vivax d- Babesia divergens
85- Balantidium coli infection may produce:
a. Frequent extra intestinal lesions
b. Rectal prolapse
c. Acute appendicitis
d. Steatorrhoea & flatulence
86- Accidental myiasis is caused by: a- Simulium
b- Culex pipiens
c- Glossina palpalis d- Musca domestica
87- All oocysts of the following parasite pass in human stool fully developed: a- Toxoplasma gondii
b- Isospora belli
c- Cryptosporidium parvum d- Cyclospora cayetanensis
88- Demodex folliculorum attacks:
a- interdigital spaces, back & axilla.
b- hair follicles & sebaceous glands.
c- pubic hairs & eye lashes.
d- inguinal region & genitalia.
89- T.cruzi can evade the immune system by: a- Antigenic modification.
b- Sequestration.
c- Cleavage of antibody molecule.
d- Ejection of membrane attack complex.
90- Epidemic relapsing fever is transmitted by: a- Saliva of body louse
b- Stool of body louse
c- Crushing of head louse d- Crushing of body louse
91- Pediculus humanus corporis transmits: a- Epidemic typhus
b- Endemic typhus c- Dengue fever
d- Oroya fever
92- Babesiosis is caused by:
a- Bite of female Anopheles
b- Bite of soft tick
c- Bite of hard tick
d- Congenital route
93- The following parasite can evade the immune system by sequestration:
a. b. c. d.
Schistosoma mansoni Trichuris trichiura
Giardia lamblia
Plasmodium vivax
94- Jaundice may accompany severe infection with:
a. Naegleria fowleri
b. Trichomonas vaginalis
c. Giardia lamblia
d. Balantidium coli
95- Watery diarrhoea is a clinical presentation in infection with: a- Entamoeba coli
b- Entamoeba histolytica
c- Cryptosporidium parvum d- Toxoplasma gondii
96- Hydrocephalus can occur in the following infections: a- Malignant malaria
b-Toxoplasmosis
c- Sleeping sickness
d- Naegleria encephalitis
97- Peritonitis occurs as a complication of:
a- Capillaria infection
b. Giardia lamblia infection c. Balantidium coli infection d. Trichinella infection
98- Semi-specific myiasis occurs due to invasion of human tissues by:
a. b. c. d.
Gastrophilus larva Stomoxys larva Oestrus larva Wohlfahrtia larva
99- Phthirus pubis is found attached to:
a. b. c. d.
aural hairs of patients nasal hairs of patients sole of foot of patient eye lashes of patients
100- Trans-ovarian transmission occurs in:
a. b. c. d.
Human fleas Metallic flies
Hard ticks
Mosquitoes
101- The following protozoon is sexually transmitted to man: a- Plasmodium ovale
b- Balantidium coli
c- Giardia lamblia
d- Trichomonas vaginalis
102- Semi-specific myiasis occurs due to invasion of human tissues by:
a.
b.
c. d.
Larva of Oestrus ovis Larva of Calliphora Larva of Aedes aegypti Larva of Cordylobia
103- Vagabond’s disease occurs due to: a- Heavy infection with bed bugs
b- Heavy infection with lice
c- Heavy infection with fleas
d- Heavy infection with storage mites
104- Diagnosis of myiasis depends on: a- Severity of the case
b. c. d.
Size of the invading larvae
Site of the lesion
Identification of posterior spiracles
105- Tick paralysis occurs due to:
a- Viral infection transmitted by soft ticks.
b- Bacterial infection transmitted by soft ticks. c- Toxins released by ticks in their saliva.
d- Toxins released by ticks in their stool.
106- Metronidazole is NOT indicated in the treatment of: a-Trichomonas vaginalis
b- Entamoeba histolytica c- Acanthamoeba
d- Balantidium coli
107- The infective stage of visceral leishmaniasis is:
a.
b. c. d.
The promastigote form
The epimastigote form
The amastigote form The trypomastigote form
108- A flask-shaped ulcer develops in the following protozoal infection: a- Leishmania infection
b- Isospora belli infection c-Cryptosporidium parvum infection d- Balantidium coli infection
109- Severe Giardiasis occurs in patients with:
a. b. c. d.
a- blood film examination shows pigments in infected RBCs. b- infection occurs by soft tick bite.
c- Infection is severe in immunocompromized patient.
d- periodicity of symptoms occur.
111- Body louse transmits B.recurrentis by: a- its release in saliva
b- its release in faeces
c- its release in crushed body
d- its release in coxal fluid
112- Adherence of the parasitized red cells in P. falciparum infection is the cause of: a- black water fever
b- malarial recrudescence
c- cerebral malaria
d- malarial relapse
113- Human flea transmits plague to man by:
a- inoculating Yersinia pestis by posterior station
Increased secretory IgA in small intestine Hypergammagloulinaemia
Increased gastric acidity
Diminished gastric acidity or achlorohydria 110- In human infection with Babesia, the following is true:
b- inoculating Yersinia pestis by anterior station c- inoculating Yersinia pestis by crushing of flea d- inoculating Yersinia pestis in coxal fluid
114- Body louse transmits R.prowazekii by: a- anterior station
b- posterior station
c- trans-ovarian route
d- release in coxal fluid
115- Perennial rhinitis may be caused by: a- Storage mites
b- House dust mites
c- Itch mites
d- Trombiculate mites
116- Recrudescence occurring in P.malariae & P.falciparum is due to: a- low grade parasitaemia with lowered immunity.
b- reactivation of hypnozoites in the liver.
c- Hepatocytes rupture & release of schizont content.
d- Formation of gametocytes in blood stream.
117- Rickettsia prowazekii:
a-Is transmitted in epidemic by tick bite. b-Remain dormant to cause Brill Zinsser disease. c-Multiplies in the body cavity of body louse.
d-Is transmitted in the saliva of body louse.
118- Nephrotic syndrome in quartan malaria is due to: a- Autoimmune reaction.
B-Immune complex deposition.
c- Granuloma formation.
d- Immunosuppression.
119- L. donovani ( visceral leishmaniasis or kala azar ) produces the following immunopathological lesion in patient’s body:
a- Autoimmune reaction.
b- Granuloma formation.
c- Immune complex deposition. d- Immunosuppression.
120- P.falciparum produces the following immunopathological lesion in patient’s body: a- Autoimmune reaction.
b- Granuloma formation.
c- Immune complex deposition. d- Immunosuppression.
121- Specific myiasis occurs due to invasion of human tissues by:
a.
b.
c.
d.
Piophila larva Dermatobia larva Stomoxys larva Wohlfahrtia larva
122- Itch mite( scabies ) produces the following skin lesion:
a. acne-like lesions & comedones.
b. elevated reddish tracks with minute vesicles.
c. nodular lesions at bony prominences
d. depigmented & hyperpigmented skin areas.
123- Follicle mite ( demodex) produces the following skin lesion: a- acne-like lesions & comedones.
b- elevated reddish tracks with minute vesicles. c- nodular lesions at bony prominences
d- depigmented & hyperpigmented skin areas.
124- Q-fever is transmitted through: a.Saliva of ticks
b.Stool of ticks
c- Saliva & stool of ticks d- Crushing of tick
125- In granulomatous amoebic encephalitis:
a- Infection is strongly associated with swimming.
b- Primary infection occurs in upper respiratory tract. c- Diffuse meningo-encephalitis is common.
d- Invasion of CNS is secondary to primary infection.
126- Water-borne protozoal infection includes: a- Chagas’ disease
b- Trichomoniasis
c- Leishmaniasis
d- Cryptosporidiosis
127- Enlargement of lymph nodes does not occur in: a- African trypanosomiasis
b- Balantidiasis
c- Toxoplasmosis
d- Kala azar
128- The patient passes stool containing mucus tinged with blood in: a-Entamoeba histolytica infection
b-Trichomonas vaginalis infection c-Giardia lamblia infection
d- Toxoplasma gondii infection
129- Duodenitis may occur in the following parasitic infection: a-Trichuriasis
b- Strongyloidiasis c- Amoebiasis
d- Giardiasis
130- The following is not an example of immunopathological reaction to parasitic infections: a-Occurrence of Katayama syndrome
b- Occurrence of nephrotic syndrome
c- Occurrence of amoebic liver abscess
d- Occurrence of black water fever
131- Inhibition of macrophage activity occurs in infection with: a-Babesia divergens
b-Trypanosoma gambiense
c- Leishmania donovani
d- Plasmodium malariae
132- Inhibition of macrophage activity occurs in infection with:
a- Babesia microti
b- Entamoeba histolytica c- Trypanosoma cruzi
d- Plasmodium vivax
133- Inhibition of macrophage activity occurs in infection with:
a- Toxoplasma gondii
b- Giardia lamblia
c- Trypanosoma rhodesiense e- Plasmodium falciparum
MCQ
1- Trophozoite form of amoeba are most likely to be found in :-
a- Semi-formed stool
b- Hard stool
c- Diarrheal stool
d- All of the above
2- Trichomonas vaginalis is least likely to be recovered from:-
a- Urine
b- Vaginal discharge
c- Urethral discharge
d- Feces
3- The amoeba having a flagellate form is :-
a- Trichomonas vaginalis
b- Naegleria fowleri
c- Acanthamoeba
d- All of the above
4- The flagellate without cyst stage is :-
a- Balantidium coli
b- Trichomonas vaginalis ( or dientamoeba fragilis , trichomonas hominis , trichomonas tenax)
c- Giardia lamblia
d- Entamoeba coli
5- All these are pathogenic protozoa except :-
a- Entamoeba histolytica
b- Entamoeba coli ( OR E. hartmanii , E.dispar )
c- Balantidium coli
d- Giardia lamblia
6- Which of the following cause primary amoebic encephalitis ( PAM) :-
a- Entamoeba histolytica
b- Dientamoeba fragilis
c- Naegleria fowleri
d- Balantidium coli
7- Which of the following protozoa is not transmitted by contaminated food or drink :-
a- Giardia lamblia
b- Trichomonas vaginalis
c- Entamoeba histolytica
d- Balantidium coli
8- The amoebic liver abscess :-
a- Associated with eosinophilia
b- Associated with lymphadenopathy
c- Associated with portal HTN
d- Should be aspirated , reveals anchovy sauce appearance
9- The following statement concerning giardia are true except :-
a- Infection is usually acquired by ingestion of food or drink
b- Causes malabsorption and steatorrhea
c- Autoinfection is common
d- Infective stage is trophozoite
10- Each of the following statements concerning trichomonas vaginalis is correct except :-
a- T.vaginals is transmitted sexually
b- T.vaginals cab be diagnosed by visualizing trophozoite
c- T.vaginals can be treated by metronidazole ( flagyl)
d- T.vaginals causes bloody diarrhea
11- Charcot leyden crystals appear in stool in infection with :-
a- Entamoeba histolytica
b- Entamoeba coli
c- Bacillary dysentery
d- Trichomonas vaginalis
12- Contaminated green salad may cause infection with :-
a- Entamoeba histolytica
b- Balantidium coli
c- Giardia lamblia
d- All of the above
13- Balantidium coli infection may produce
a- Extra- intestinal lesions
b- Acute appendicitis
c- Rectal prolapse
d- Steatorrhea & flatulence
14- Jaundice may accompany severe infection with :-
a- Naegleria fowleri
b- Trichomonas vaginalis
c- Giardia lamblia
d- Balantidium coli
15- Dental caries may accompany with :-
a- Trichomonas vaginalis
b- Trichomonas hominis
c- Trichomonas tenax
d- Dientamoeba fragilis
16- The following protozoan transmit sexually to man :-
a- Trichomonas vaginalis
b- Trichomonas hominis
c- Trichomonas tenax d-Giardia lamblia
17- Metronidazole is not indicated in treatment of :-
a- Trichomonas vaginalis
b- Entamoeba histolytica
c- Balantidium coli
d- Acanthamoeba
18- A flask shaped ulcer develop in :-
a- Entamoeba histolytica
b- Balantidium coli
c- Giardia lamblia
d- A,b
19- Severe giardiasis occur in patient with :-
a- Hypergammaglobunaemia
b- Increased secretory IgA in small intestine
c- Increased gastric acidity
d- Diminished gastric acidity or achlorohydria
20- The patient pass stool with mucous tinged with blood in :-
a- Entamoeba histolytica infection
b- Trichomonas vaginalis infection
c- Giardia lamblia infection
d- Trichomonas vaginalis infection
21- The following protozoan can detect in urine :-
a- Trichomonas vaginalis trophozoite
b- Trichomonas vaginalis cyst
c- Giardia lamblia cyst
d- Chilomastix menslii cyst
22- Normal habitat of chilomastix menslii is :-
a- Mouth
b- Large intestine
c- Small intestine
d- Urogenital tract
23- Stool in bacillary dysentery is:-
a- Bulky & offensive
b- Alkaline
c- Acidic
d- Contain charcot leyden crystals
24- Stool in amebic dysentery is :-
a- Bulky & offensive & acidic
b- Bulky & offensive & alkaline
c- Contain bacteria
d- Contain numerous altered RBCs & pus cells
25- Infection of vagina with Candida albicans:-
a- Occur in Alkaline PH of vagina
b- Occur in Acidic PH of vagina
c- Treated with metronidazole
d- Cause fishy odour
MCQ
26- Trophozoite form of amoeba are most likely to be found in :-
e- Semi-formed stool
f- Hard stool
g- Diarrheal stool
h- All of the above
27- Trichomonas vaginalis is least likely to be recovered from :-
e- Urine
f- Vaginal discharge
g- Urethral discharge
h- Feces
28- The amoeba having a flagellate form is :-
e- Trichomonas vaginalis
f- Naegleria fowleri
g- Acanthamoeba
h- All of the above
29- The flagellate without cyst stage is :-
e- Balantidium coli
f- Trichomonas vaginalis ( or dientamoeba fragilis , trichomonas hominis , trichomonas tenax)
g- Giardia lamblia
h- Entamoeba coli
30- All these are pathogenic protozoa except :-
e- Entamoeba histolytica
f- Entamoeba coli ( OR E. hartmanii , E.dispar )
g- Balantidium coli
h- Giardia lamblia
31- Which of the following cause primary amoebic encephalitis ( PAM) :-
e- Entamoeba histolytica
f- Dientamoeba fragilis
g- Naegleria fowleri
h- Balantidium coli
32- Which of the following protozoa is not transmitted by contaminated food or drink :-
e- Giardia lamblia
f- Trichomonas vaginalis
g- Entamoeba histolytica
h- Balantidium coli
33- The amoebic liver abscess :-
e- Associated with eosinophilia
f- Associated with lymphadenopathy
g- Associated with portal HTN
h- Should be aspirated , reveals anchovy sauce appearance
34- The following statement concerning giardia are true except :-
e- Infection is usually acquired by ingestion of food or drink
f- Causes malabsorption and steatorrhea
g- Autoinfection is common
h- Infective stage is trophozoite
35- Each of the following statements concerning trichomonas vaginalis is correct except :-
e- T.vaginals is transmitted sexually
f- T.vaginals cab be diagnosed by visualizing trophozoite
g- T.vaginals can be treated by metronidazole ( flagyl)
h- T.vaginals causes bloody diarrhea
36- Charcot leyden crystals appear in stool in infection with :-
e- Entamoeba histolytica
f- Entamoeba coli
g- Bacillary dysentery
h- Trichomonas vaginalis
37- Contaminated green salad may cause infection with :-
e- Entamoeba histolytica
f- Balantidium coli
g- Giardia lamblia
h- All of the above
38- Balantidium coli infection may produce
e- Extra- intestinal lesions
f- Acute appendicitis
g- Rectal prolapse
h- Steatorrhea & flatulence
39- Jaundice may accompany severe infection with :-
e- Naegleria fowleri
f- Trichomonas vaginalis
g- Giardia lamblia
h- Balantidium coli
40- Dental caries may accompany with :-
e- Trichomonas vaginalis
f- Trichomonas hominis
g- Trichomonas tenax
h- Dientamoeba fragilis
41- The following protozoan transmit sexually to man :-
d- Trichomonas vaginalis
e- Trichomonas hominis
f- Trichomonas tenax
g- Giardia lamblia
42- Metronidazole is not indicated in treatment of :-
e- Trichomonas vaginalis
f- Entamoeba histolytica
g- Balantidium coli
h- Acanthamoeba
43- A flask shaped ulcer develop in :-
e- Entamoeba histolytica
f- Balantidium coli
g- Giardia lamblia
h- A,b
44- Severe giardiasis occur in patient with :-
e- Hypergammaglobunaemia
f- Increased secretory IgA in small intestine
g- Increased gastric acidity
h- Diminished gastric acidity or achlorohydria
45- The patient pass stool with mucous tinged with blood in :-
e- Entamoeba histolytica infection
f- Trichomonas vaginalis infection
g- Giardia lamblia infection
h- Trichomonas vaginalis infection
46- The following protozoan can detect in urine :-
e- Trichomonas vaginalis trophozoite
f- Trichomonas vaginalis cyst
g- Giardia lamblia cyst
h- Chilomastix menslii cyst
47- Normal habitat of chilomastix menslii is :-
e- Mouth
f- Large intestine
g- Small intestina
h- Urogenital tract
48- Stool in bacillary dysentery is :-
e- Bulky & offensive
f- Alkaline
g- Acidic
h- Contain charcot leyden crystals
49- Stool in amebic dysentery is :-
e- Bulky & offensive & acidic
f- Bulky & offensive & alkaline
g- Contain bacteria
h- Contain numerous altered RBCs & pus cells
50- Infection of vagina with Candida albicans:-
a- Occur in Alkaline PH of vagina
b- Occur in Acidic PH of vagina
c- Treated with metronidazole
d- Cause fishy odour
51- Trophozoites are infective stage in :-
a- E. histolytica b- E.coli
c- T.vaginalis d- E.dispar
52- Winterbottom’s sign is seen in :-
a- toxoplasmosis b-leishmania
c-african trypanososmes d-acute chagas’ disease
53- The following arthropod transmit cutaneous leishmaniasis :-
a- aedes b-glossina c-phlebotomus d-simulium
54- The following arthropod can transmit leishmania tropica minor ( L.tropica ) :-
a- glossina palpalis b-glossina morsitans c-aedes
d-stomoxys calcitrans
55- Salivary glands are devoid from parasitic forms in :-
a- glossina palpalis b-glossina morsitans c-lutzomyia
d-tunga penetrans
56- Proboscis of arthropod can transmit :-
a- Gambian sleeping sickness b-chagas’ disease
c-kala- azar
d-rhodesian sleeping sickness
57- In diagnosis of cutaneous leishmaniasis , biopsy is taken from :-
a-base of ulcer
b-edge of ulcer
c-skin around ulcer
d-lymph node draining ulcer
58- Best diagnosis of kala- azar ( visceral leishmaniasis ) , we depend on :-
a- detect parasites in blood film
b-biopsy from bone marrow to detect amastigotes
c-serological test
d-montenegero test
59- Leismania tropica ulcer left untreated , the following occurs :-
a-spreading to m.m.
b-development of disfiguring ulcer & solid immunity
c-spreading erode cartilage
d-ulcer heal leave no scar
60- In granulomatous amoebic encephalitis :-
a- infection is strongly associated with swimming
b-primary infection occur in upper respiratory tract
c-diffuse meningo-encephalitis is common
d-invasion of CNS is secondary to primary infection
61- Enlargement of LNs doesn’t occur in :-
a- African trypanososmes b-kala azar c-balantidiasis
d-chagas’ disease
62- Oriental sore is caused by bite of :-
a- glossina species b-phlebotomus species c-stomoxys calcitrans d-a,c
63- Xenodiagnoses can be applied for diagnosis of :- a-L.donovani
b-T.cruzei
c-L.tropica
d-T.brucei
64- In visceral leishmaniasis , culture on NNN medium results in
a- amastigote
b-promastigote ( leptomonad form )
c-epimastigote
d-leishmanoid form
65- Drug of choice in ttt of primary amebic encephalitis is :- a- amphotericicn B
b- metronidazole
c-tinidazole
d-nifurtimox
66- Pathogenic species of trypanosoma that is present in America are :-
a- T.gambiense
b-T. rhodesiense
c-T.cruzi
d-none of the above
67- Principal insect vector of T.rhodesiense is :-
a-triatoma b-sandfly c-tse tse
d- mosquitoes
68- Protozoa causing conjunctivitis include :- a-T.cruzi
b-T.brucei c-L.donovani d-none of the above
69- The characteristic romana’s sign is in :-
a-leishmaniasis b-toxoplasmosis c-sleeping sickness d-acute chagas’ disease
70- Which of the following protozoa primarily infect macrophages
a-T.brucei b-T. cruzei c-L.donovani d-T. vaginalis
1-The following are anatomic structures of the auricle except :
a- Helix
b-Tragus
c-Concha
d-Antrum
( The antrum is the largest air cells of the mastoid bone )
2-The auriculo temporal nerve
a-supplies the skin of the upper 2/3 of the lateral surface of the auricle b- is a branch of maxillary nerve
c- supplies the middle ear mucosa through the tympanic plexus
d- non of the above
-The auriculo-temporal nerve is a branch of mandibular division of the trigeminal nerve
- The middle ear mucosa is supplied by the tympanic branch of Glosspharyngeal nerve called Jacobson nerve
3-The lobule of the ear has its sensory innervation from:
a-great auricular nerve
b- auriculotemporal nerve c-arnold branch of vagus d- facial nerve
4-The tympanic membrane is divided into:
a- Two equal parts called pars tensa and pars flaccida
b- A major upper part called pars flaccida and a small lower part called pars tensa c-A small upper part called pars flaccida and a major lower part called pars tensa d- non of the above
5-The bulge seen on the medial wall of the middle ear is :
a- known as the promontory
b- formed by the bony semicirculr canal
c-is formed by the basal turn of the bony cochlea d-all of the above
e- both 1 and 2
f- both 1 and 3
6-The Eustachian tube is opened by contraction of :
a- tensor tympani muscle b-levator palati muscle c-tensor palati muscle d-Salpingopharyngeus muscle
7-The sensory end-organ of the semicircular canal is :
a- the organ of Corti b- the macula c- the crista
d- non of the above
-The organ of Corti is the sensory end organ of hearing in the cochlea -The macula is the sensory end organ in the utricle and saccule
8-Auricular hematoma
a- may be complicated by otitis externa
b- cauli ear is one of its complications
c- evacuation of the extra-vasated blood is not essential
d- all of the above
-Auricular hematoma may be complicated by perichondritis and
cauli ear
evacuation of the extra-vasated blood is essential to avoid complications
9-It is better to avoid ear wash for removal of :
a- wax
b- animate foreign body
c- impacted vegetable foreign body
d- non of the above - Vegetable FB will swell if ear wash fails to get it out which will cause more impaction
10-It is better to avoid ear wash for removal of :
a- wax
b- animate foreign body
c-calculator battery
d- non of the above
-Don’t wash if the FB is a calculator battery as this may lead to leak of acid and chemical burn of the skin
11-The causative organism in ear fruncle is :
a- proteus
b- Pseudomonas c- staph. Aeureus d- E coli
12-The causative organism in malignant otitis externa :
a- proteus b-Pseudomonas c-staph. Aeureus
d- morexella catarrhalis
13-Malignant otitis externa is :
a- a truly malignant disease eroding the external canal
b- is most commonly seen in elderly uncontrolled diabetics c- staphylococcus aureus is the causative organism
d- non of the above 14-In the adult, the Eustachian tube is approximately the following lehgth :
a- 30 mm b- 20 mm c- 36 mm d- 45 mm
15-In Gradenigo syndrome diplopia is due to inflammation of the following cranial nerve :
a- IV nerve
b- V nerve
c- III Nerve
d- VI nerve
-This syndrome is charecterized by: 1- otorrhoea
2-facial pain due to iritation of V cranial nerve
3-diplopia and squint due to iritation of VI cranial nerve in Dorello canal
16-Conductive deafness in longtudinal temporal bone fracture may be due to:
a- Rupture of the tympanic membrane b- Ossicular disruption
c- Non of the above
d- Both 1 and 2
17-Longtudinal temporal bone fracture :
a- is less common than the transverse type
b- is usually associated with sensori-neural hearing loss
c- facial nerve paralysis is a common association with this type d- non of the above
18-The following organisms are involved in acute otitis media except
a- streptococcus pneumonia b-hemophilus influenza c-Pseudomonas aeroginosa d-morexella cararrhalis
19-All of the following are diagnostic of tympanic membrane retraction except
a- fore-shortened handle of malleus
b- prominent lateral process of malleus
c- Schwartz sign
d- distorted cone of light
-Schwartz sign is a flamingo red tinge of the tympanic membrane due to increased vascularity of the promontory and indicates active otosclerosis
20-Throbbing and severe earach is present in the following stage of acute otitis media :
a- stage of salpingitis
b- stage of catarrhal otitis media
c- stage of suppurative otitis media
d- stage of tympanic membrane perforation 21-The tympanic membrane perforation in acute otitis media is
a- central in the pars tensa b- marginal in the pars tensa c- small in the pars flaccida d- non of the above
22-Type c tympanogram is consistent with :
a- secretory otitis media
b- otosclerosis
c- Eustachian tube dysfunction
d- otosclerosis
-In Type C there is Normal compliance but the peak of the tympanogram is at the negative side so it is consistent with ET dysfunction in which there is negative pressure in the middle ear
23-By central drum perforation we mean :
a- a perforation at the central part of the drum
b- a perforation in the pars tensa which is surrounded by a rim of tympanic membrane c a perforation of the pars flaccida
d- a perforation in the pars tensa which is not surrounded by a rim of tympanic membrane
24-All of the following may be seen in the tubotympanic type of chronic suppurative otitis media except
a- mucopurulent otorrhoea
b- central tympanic membrane perforation
c- marginal tympanic membrane perforation d- profuse otorrhoea
25-Cholesteatoma is characterized by
a- continuous mucopurulent ear discharge b-A foul smelling ear discharge
c- A central tympanic membrane perforation d- non of the above
26-A child with retraced drum and conductive deafness after inadequate treatment of acute suppurative otitis media is suffering from :
a-chronic tubotympanic otitis media
b-chronic atticoantral otitis media
c- otitis media with effusion d- all of the above
e-non of the above
27-The commonest cause of conductive deafness in children is:
a- wax
b-secretory otitis media c-otomycosis
d- otosclerosis
28-The commonest cause of conductive deafness in adults is: a- wax
b-secretory otitis media c-otomycosis
d- otosclerosis
29-In a patient suffering from purulent otorrhoea and attic perforation :
a- treatment is essentially surgical
b- medical treatment and follow up is sufficient
c- myringoplasty is the only needed treatment
d- non of the above
-The presence of foul odour otorrhoea and attic perforation is diagnostic of cholesteatoma. Treatment of this case is essentially surgical by mastoidectomy operation ( radical or modified radical)
30-In a 45 years old female patient presenting with pulsating tinnitus and red mass behind the drum, all of the following are true except :
a- glomus tumour is a possible diagnosis
b-more assessment is needed by CT scan or MRI
c- MRI angiography confirm the diagnosis
d-biopsy is essential to verify the pathological nature -Biopsy is contraindicated as it will lead to profuse bleeding
31-Bezold abscess is a collection of pus :
a- above and in front of the auricle
b-behind the auricle
c-in the upper part of the neck deep to the sternomastoid d- in the peritonsillar space
32-During ear examination the reservoir sign is diagnostic of:
a- acute otitis media b- mastoiditis
c- petrositis
d- cholesteatoma
33-An early and diagnostic sign of mastoiditis is :
a- reservoir sign
b-sagging of the posterosuperior part of the bony canal
c-perforated tympanic membrane
d- postauricular mastoid abscess
-Sagging means bulging downwards of the posterosuperior part of the bony external canal and is due to periostitis of the bone overlying the mastoid antrum. It is an early and diagnostic sign of mastoiditis
34-Vertigo and nystagmus induced by pressure on the tragus is diagnostic of :
a- serous labyrinthitis
b- circumscribed per- labyrintserous c suppurative labyrinthitishitis
d all of the above
35-In a case of cholesteatoma, sever spontaneous vertigo with Nausea and vomiting is suspicious of
a- circumscribed peri-labyrinthitis b- diffuse serous labyrinthitis
c- extradural abscess
d- petrositis
36-In a patient having acute suppurative otitis media with bulging drum, myringotomy is benificial to
a-drain the middle ear
b- avoid rupture of the tympanic membrane
c-avoid complications d-all of the above
37-The most common complication of myringotomy operation is
a- injury of facial nerve b-dislocation of the incus c-injury of the jagular bulb d- residual perforation
38-In myringotomy operation the posterosuperior quadrant of the tympanic membrane must be avoided :
a- to avoid injury of dehiscent jagular bulb
b- to avoid injury of the ossicles
c- non of the above d- both 1 & 2
39-The combination of unilateral otorrhoea, severe facial pain and diplopia is known as :
a- Piere Robin syndrome
b- Gradenigo’s syndrome
c- Kartagner syndrome
d- Ramsay Hunt sundrome
40-A child with an attic drum perforation who developed nausea, projrctile vomiting and fever of 40 degree is suspicious to have got :
a- otogenic meningitis
b- otogenic labyrinthitis
c- petrositis d- mastoiditis
41-The first line of treatment in a child who develops lower motor neurone facial paralysis after acute otitis media is :
a- antibiotics and corticosteroids
b- decompression of facial nerve
c- exploration of facial nerve d- myringotomy
42-Intermittent fever with rigors and headach in a patient with cholesteatma may be due to :
a-otogenic meningitis b-otogenic brain abscess
c- lateral sinus thrombophlebitis d-extradural abscess
43-A positive Kernig sign means
a-reflex flexion of the hips and knees when the neck is flexed
b- inability to extend the knee completely when the hip is flexed on the abdomen c- inability to do rapid ulternating movement
d- non of the above
44-A positive Brudzniski sign means
a-reflex flexion of the hips and knees when the neck is flexed
b- inability to extend the knee completely when the hip is flexed on the abdomen c- inability to do rapid ulternating movement
d- non of the above
45-A persistent profuse ear discharge after acute otitis media is
a- cholesteatoma
b- secretory otitis media
c-mastoiditis
d- diffuse otitis externa
-in mastoiditis there is profuse mucopurulent or purulent otorrhoea which recurs rapidly after remova ( a diagnostic sign called reservoir sign)
46-In otitic barotrauma, the following statements are correct except:
a-occurs during airplane ascent
b- occurs during airplane rapid descent
c- can cause rupture of the tympanic membrane d- occurs during diving
47-The commonest cause of vertigo is
a- meniere’s disease
b-labyrinthitis
c-benign paroxysmal positional vertigo d-ototoxicity
48-Most cases of extradural abscess of the temporal lobe
a- are asymptomatic and discovered accidentally during mastoidectomy b- present with persistent ipsilateral temporal headach
c- present with vertigo
d- present with pulsating discharge,hearing loss and tinnitus
49-The type of hearing loss in otosclerosis may be
a- conductive
b- sensorineural c-mixed
d-all of the above -In stapedial otosclerosis hearing loss is conductive -In cochlear type the hearing loss is sensorineural -In combined otosclerosis the hearing loss is mixed
50-The commonest cause of bilateral sensorineural hearing loss in elderly individuals is
a- cochlear otosclerosis
b- presbyacusis
c- diabetes milltus d- ototoxicity
51-A 30 years old patient with recurrent attacks of vertigo, hearing loss and tinnitus associated with nausea and vomiting has
a- benign paroxysmal positional vertigo
b-vestibular neuronitis
c-Meniere’s disease d-acoustic neuroma]
explanation
1- In benign paroxysmal positional vertigo there is recurrent attacks of vertigo for seconds which occurs when the patient assumes certain head position
2- in vestibular neuronitis there is sudden severe vertigo for dayes but bo hearing loss 3- in Meniere’s disease recurrent attacks of vertigo, hearing loss and tinnitus associated with nausea and vomiting
52-Before tympanoplasty in a 30 years old patient, the following is required
a- audiogram
b- ensure dry perforation
c-treatment of any underlying nasal or paranasal sinus infection d-all of the above
e- non of the above
53-The XI, X and XI cranial nerves may be involved in all of the following except
a-acoustic neuroma
b-transverse temporal bone fracture
c-malignant otitis externa
d- squamous cell carcinoma of the middle ear
-in transverse temporal bone fracture the involved nerves are VII & VIII
54-In lower motor neurone facial paralysis with intact taste sensation at the anterior 2/3 of the tongue, the level of the lesion is :
a- in the internal auditory canal
b-in the horizontal tympanic part
c- in the vertical part above the stapes d- in the stylomastoid foramen
55-Failure to close the eye voluntarily is a symptom of
a- paralysis of the trigeminal nerve b- upper motor neurone facial paralysis c- lower motor neurone facial paralysis d- non of the above
56-Uncontrolled diabetes in elderly patient may predispose to
a- cholesteatoma
b- malignant otitis externa c- presbyacusis
d- vestibular neuronitis
57-A large near total perforation following acute necrotizing otitis media must be followed up for fear of
a- recurrent middle ear infection
b- secondary acquired cholesteatoma
c-retraction pocket d-tympanosclerosis
58-By modified radical mastoidectomy we mean
a- removal of mastoid air cells and all middle ear contents
c- removal of diseased mastoid air cells
c- removal of mastoid air cells and all middle ear contents with preservation of healthy remnants of tympanic membrane and ossicles
d- non of the above
59-By radical mastoidectomy operation we mean
a- removal of mastoid air cells and all middle ear contents except stapes
b- removal of diseased mastoid air cells
c- removal of mastoid air cells and all middle ear contents with preservation of healthy remnants of tympanic membrane and ossicles
d- non of the above
60-Extensive cholesteatoma is best treated by
a- cortical mastoidectomy
b- radical mastoidectomy
c- modified reducal mastoidectomy
d- myringotomy wiyh insertion of T tube
61-Which of the following statements is false concerning Cochlear implant
a-postlingually deaf get far better benefit than prelingually deaf
b-it is indicated in total sensory hearing loss
c-the auditory nerve should be intact
d- After the operation speech discrimination is good and lip reading is not needed
62-Which of the following statements is wrong concerning myringotomy Operation :
a- it is indicated in acute suppurative otitis media with bulging drum
b- it is indicated in secretory otitis media after failure of medical Treatment
c- it is better done in the postero superior quadrant of the tympanic membrane d-residual perforation of the tympanic membrane is one of its complications 63-Etiology for pulsatile tinnitus includes the followings except:
a) Arteriovenous malformation of neck. b) Otosclerosis.
c) Glomus jugulare tumors.
d) Hyperthyroidism.
e) Atherosclerosis.
64-Which of the following drugs are known to cause tinnitus?
a-Salicylates. b-Loop Diuretics. c-Aminoglycosides. d-NSAID.
e-All of the above
65-Which of the following is associated with objective tinnitus
a-Menière’s disease. b-Ear wax impaction. c-Acoustic neuroma. d-Palatal myoclonus. e-Middle ear effusion
66-The following have an ototoxic effect except
a- gentamycin b- frusemide
c- streptomycin d- amoxicilline e- quinine
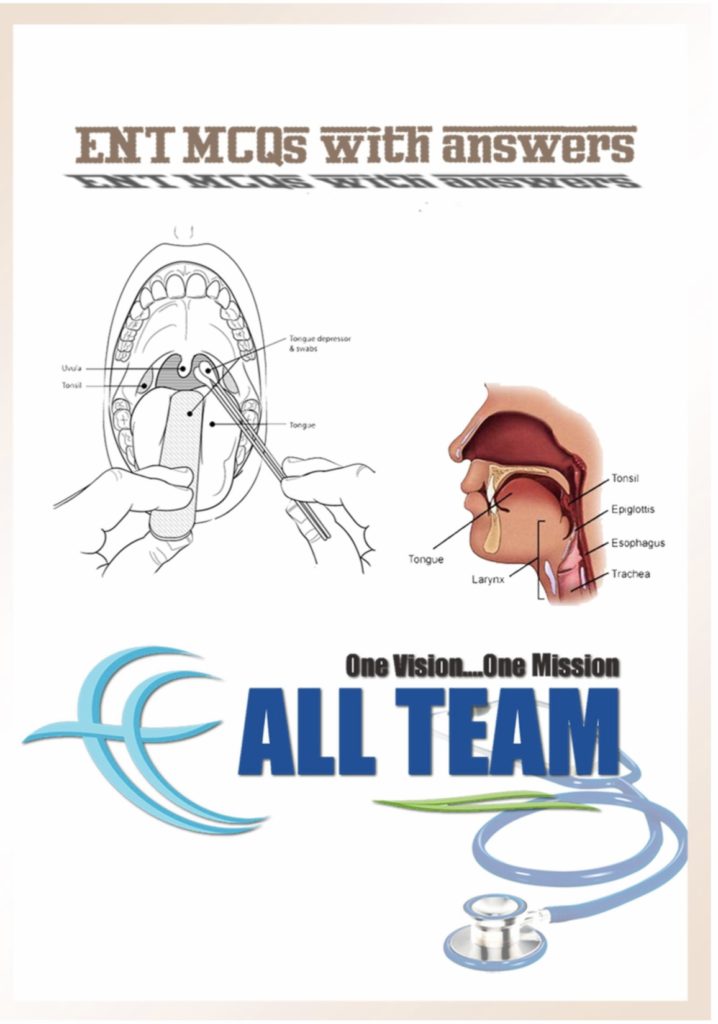
All team “One vision … One Mission” 0
The Ear
- The Following is true about the tympanic membrane EXCEPT:
a. It is rounded in shape.
b. It is placed obliquely forming acute angle with meatus anteriorly and obtuse
one posteriorly.
c. The normal tympanic membrane is pearly white in color.
d. The light reflex is due to the concave position of the membrane. - The following is true about the Eustachian tube EXCEPT:
a. It ends 1 cm behind the posterior end of the inferior turbinate.
b. The upper 1/3 is bony while the lower 2/3 is fibrocartilagenous.
c. It is normally opened at rest. - Choose the correct answer:
a. Ear washing is not contraindicated in traumatic perforation of the drum.
b. Pathological perforation of the drum occurs at any site while traumatic ones
occurs in pars tensa only.
c. In ear washing, the sterile nozzle of the syringe is directed to the drum
directly.
d. Ear washing is indicated in the presence of fistula between the middle & inner
ear. - Pain on mastication is present in:
a. Acute mastoiditis.
b. Otosclerosis.
c. Furunculosis of the external ear.
d. Allergic otitis externa. - Sagging of the postero-superior wall of the EAC occurs in:
a. Acute mastoiditis.
b. Furunculosis of the external ear.
c. Otitis media.
d. Petrositis. - The causative agent in otomycosis is:
a. Aspergillus nigers & / or Candida albicans.
b. Streptococci.
c. Staphylococci.
d. E.coli
e. B. pyocyaneus. - Ramsy-Hunt syndrome is:
a. Herpes-zoster affection of the geniculate ganglion of the facial nerve.
b. Dysphagia in middle aged female.
c. Dysphagia in old male.
d. Sensory-neural deafness in newly born. - Stapedectomy is one line for treatment of:
a. Otosclerosis.
b. Otomycosis.
c. Otitic barotrauma.
d. Secretory otitis media.
All team “One vision … One Mission” 1 - Bloody discharge from the ear occurs in:
a. Fracture base of the skull.
b. Glomus jugular tumor.
c. Haemorrhgic otitis media.
d. Rupture drum.
e. All of the above.
f. Non of the above. - The most common cause of deafness in children:
a. Acute otitis media.
b. Secretory otitis media.
c. Chronic otitis media.
d. Cholesteatoma. - In traumatic ossicular disruption, all is true EXCEPT:
a. The audiogram shows 55 dB loss.
b. Separation of the icudo-stapedial joint is the commonest lesion.
c. There is bulging drum.
d. C.T scan is indicated. - Crescentic hairline is an otoscopic finding in:
a. Otomycosis.
b. Otosclerosis.
c. Secretory otitis media.
d. Acute otitis media. - Reservoir is a characteristic sign in:
a. Acute mastoid abscess.
b. Acute otitis media.
c. Chronic otitis media.
d. Secretory otitis media. - Gradinigo syndrome occurs in:
a. Acute mastoid abscess.
b. Acute petrositis.
c. Chronic otitis media.
d. Secretory otitis media. - Griesinger’s sign is:
a. Edema & tenderness over the posterior border of the mastoid process.
b. Unilateral pulsating otorrhoea.
c. Vertigo & nystagmus on increasing the pressure of the EAC.
d. Tenderness on the tip of mastoid bone. - Fever in lateral sinus thrombosis is:
a. Intermittent.
b. Remittent.
c. Low grade.
d. High grade.
All team “One vision … One Mission” 2 - Tobey-Ayer’s test is a characteristic sign in:
a. Brain abscess.
b. Lateral sinus thrombosis.
c. Extradural abscess.
d. Meningitis.
e. Cavernous sinus thrombosis. - Pain in acute tonsillitis is referred to the ear through:
a. The 5th nerve.
b. The 9th nerve.
c. The 10th nerve.
d. 2nd & 3rd cervical nerve. - Pain in acute sinusitis is referred to the ear through:
a. The 5th nerve.
b. The 9th nerve.
c. The 10th nerve.
d. 2nd & 3rd cervical nerve. - Pain in tempro-mandibular joint is referred to the ear through:
a. The 5th nerve.
b. The 9th nerve.
c. The 10th nerve.
d. 2nd & 3rd cervical nerve. - Pain in cancer larynx is referred to the ear through:
a. The 5th nerve.
b. The 9th nerve.
c. The 10th nerve.
d. 2nd & 3rd cervical nerve. - Pain in salivary calculi is referred to the ear through:
a. The 5th nerve.
b. The 9th nerve.
c. The 10th nerve.
d. 2nd & 3rd cervical nerve. - The fluids presents in secretory otitis media is:
a. Mucopurulent.
b. Serosanguinous.
c. Exudates.
d. Transudates.
e. Mixture of exudates & transudates. - The discharge in case of cholesteatoma is:
a. Copious purulent.
b. Copious offensive.
c. Scanty offensive.
d. Thick scanty creamy.
All team “One vision … One Mission” 3 - Watery discharge from the ear occurs in all of the following EXCEPT:
a. Cerebro-spinal otorrhoea.
b. Parotid fistula.
c. Acute otitis media.
d. Endolymphatic sac surgery. - In Rinne’s test:
a. In perceptive deafness: air conduction is better than bone conduction.
b. In conductive deafness: air conduction is better than bone conduction.
c. In conductive deafness: bone conduction is better than air conduction.
d. In perceptive deafness: bone conduction is better than air conduction. - In Weber’s test:
a. In conductive deafness: sound is heard better in the diseased ear.
b. In conductive deafness: sound is heard better in the healthy ear.
c. In perceptive deafness: sound is heard better in the healthy ear.
d. In perceptive deafness: sound is heard better in the diseased ear. - Schwabach’s test is:
a. Comparison between air & bone conduction of the same ear.
b. Comparison of bone conduction of both ears at the same time.
c. Comparison of duration of bone conduction of the patient & the examiner. - The following is true about pure tone audiometry EXCEPT:
a. It gives the amount of the hearing loss in dB.
b. It gives the type of deafness.
c. It gives the possible cause of deafness.
d. It helps in hearing aid selection.
e. It helps in follow up of the case.
f. It measures the sound emitted from the cochlea. - The following is true about impedance audiometry EXCEPT:
a. It measures the pressure changes in the middle ear.
b. It measures fixation and dislocation of the ossicular chain.
c. It measures the patency of the Eustachian tube.
d. It measures the sound emitted from the cochlea. - In lesion of the facial nerve at the stylomastoid foramen, there is:
a. L.M.N.L of the facial muscles.
b. No impairment of taste.
c. No impairment of salivation.
d. No impairment of lacrimation.
e. All of the above. - In lesion of facial nerve at vertical part”below the nerve of stapedius” there is:
a. Loss of taste.
b. Impairment of salivation.
c. Impairment of lacrimation.
d. Hyperacusis.
All team “One vision … One Mission” 4 - In lesion of the facial nerve at horizontal part, there is:
a. Loss of taste.
b. Impairment of salivation.
c. Impairment of lacrimation.
d. Hyperacusis.
e. All of the above. - In lesion of the facial nerve at the geniculate ganglion, there is:
a. Loss of taste.
b. Impairment of salivation.
c. Impairment of lacrimation.
d. Hyperacusis.
e. All of the above. - In UMNL of the facial nerve, there is:
a. Paralysis of the muscles of the lower 1/2 of the face on the opposite side.
b. Paralysis involves the voluntary but spares the emotional & associative
movement.
c. Hypotonia.
d. Hyporeflexia. - In LMNL of the facial nerve, there is:
a. Paralysis of the muscles of the lower 1/2 of the face on the opposite side.
b. Paralysis involves the voluntary but spares the emotional & associative
movement.
c. Hypotonia.
d. Hyporeflexia.
e. Reaction of degeneration. - In LMNL of the facial nerve, there is:
a. Paralysis of the muscles of the lower & upper 1/2 of the face on the opposite
side.
b. Paralysis involves the voluntary, emotional & associative movement.
c. Paralysis of the muscles of the lower & upper 1/2 of the face on the same side. - Bell’s palsy is LMNL at the level of:
a. Geniculate ganglion.
b. Internal facial auditory meatus.
c. Stylomastoid foramen.
d. Cerebellopontine angle. - The cause of Bell’s palsy may be one of the following EXCEPT:
a. Vascular ischemia.
b. Virus infection.
c. Bacterial infection.
d. Auto immune. - The early symptom of Bell’s palsy is:
a. Dropping of angle of the affected side.
b. Obliteration of the angle of the mouth.
c. Pain of acute onset behind the ear.
d. Inability to close the eye.
All team “One vision … One Mission” 5 - Intra cranial complications of chronic suppurative otitis media includes:
a. Mastoiditis.
b. Meningitis.
c. Labyrinthitis.
d. Brain abscess. - Cranial complications of chronic suppurative otitis media includes:
a. Mastoiditis.
b. Labyrinthitis.
c. Petrositis.
d. Facial nerve paralysis.
e. All of the above. - Extra cranial complications of chronic suppurative otitis media includes:
a. Mastoiditis.
b. Bezold abscess.
c. Lateral sinus thrombosis.
d. Otitis externa. - CSF examination in case of meningitis shows:
a. Protein diminished.
b. Sugar diminished.
c. Chloride diminished.
d. Cell count increased.
e. a, b & c.
f. b, c & d. - All are correct about Meniere’s disease EXCEPT:
a. It is an endolymphatic hydrops.
b. Males are more affected than females.
c. The type of deafness is conductive.
d. Decompression of the labyrinth is indicated if the vertiginous attack is
crippling. - The aim of radical mastoidectomy is:
a. To give safe ear.
b. To preserve hearing.
c. Reconstruct the ossicles.
d. Reconstruct the tympanic membrane. - The aim of modified radical mastoidectomy is:
a. To give safe ear & to preserve hearing.
b. Reconstruct the ossicles.
c. Reconstruct the tympanic membrane. - The pain in acute suppurative otitis media in the suppurative stage is:
a. Dull aching.
b. Throbbing.
c. Boring.
d. Burning.
All team “One vision … One Mission” 6 - The pain in acute suppurative otitis media in the catarrhal stage is:
a. Dull aching.
b. Throbbing.
c. Boring.
d. Burning. - The pain in acute suppurative otitis media is more severe at:
a. Night.
b. Morning.
c. Mid-day.
d. All the day. - The pain in acute suppurative otitis media disappear after:
a. Bulging of the drum.
b. Perforation of the drum.
c. Congestion of the drum. - In malignant otitis externa all the following is true EXCEPT:
a. It is common in old diabetic.
b. There may be facial paralysis.
c. The commonest organism is pseudomonas.
d. Mainly treated surgically. - McEwen’s triangle is the surface landmark of:
a. The tympanic part of the facial nerve.
b. Mastoid antrum.
c. Dome of the lateral semicircular canal.
d. Icudo-stapedial joint. - Longitudinal fracture of the temporal bone may be associated with all of the
following EXCEPT:
a. LMNL facial palsy.
b. Traumatic perforation of the tympanic membrane.
c. Conductive hearing loss.
d. Profound hearing loss. - The middle ear magnifies the sound:
a. 20 times.
b. 22 times.
c. 200 times.
d. 21 times. - The test of hearing in infants is:
a. Rinne test.
b. Weber test.
c. Pure tone audiometry.
d. ABR “Auditory Brain stem Response”.
All team “One vision … One Mission” 7 - ABR “Auditory Brain stem Response” is used in:
a. Test of hearing in malingering.
b. Test of hearing in retrochoclear lesion.
c. Detection of acoustic neuroma.
d. All of the above. - The following are the manifestations of temporal lobe abscess EXCEPT:
a. Hemi paresis.
b. Aphasia.
c. Convulsive fits.
d. Vertigo. - The earliest manifestation of cavernous sinus thrombosis is:
a. Fever.
b. Ptosis.
c. Proptosis.
d. Ophthalmoplegia. - In traumatic rupture of the drum, all are true EXCEPT:
a. The main treatment is conservative.
b. Local ear drops are highly indicated.
c. It heals spontaneously within 3 months.
d. It may be caused by longitudinal fracture of the temporal bone. - Early acute suppurative otitis media is manifested by:
a. Retracted tympanic membrane.
b. Aural fullness.
c. Deafness.
d. All of the above. - The pathology in case of Bell’s palsy is:
a. Facial nerve tumor.
b. Cut in the tympanic segment in the facial nerve.
c. Edema of the facial nerve inside its bony canal.
d. Hemorrhage in the facial nerve nucleus. - The most accurate diagnostic test to detect degeneration of the facial nerve:
a. Nerve excitability test.
b. Electromyography.
c. Electroneurography.
d. Stapedial reflex. - Cholesteatoma is:
a. Benign middle ear tumor.
b. Skin in a wrong place.
c. Specific middle ear granuloma.
d. Non of the above.
All team “One vision … One Mission” 8 - Bezold’s abscess is a swelling:
a. Behind the ear.
b. Below the ear in the neck.
c. Above the ear.
d. In front of the ear. - Inability to raise the eye brow & close the same eye with deviation of the angle of the mouth to the opposite side is:
a. UMNL 7th cranial nerve palsy.
b. UMNL 5th cranial nerve palsy.
c. LMNL 5th cranial nerve palsy.
d. LMNL 7th cranial nerve palsy. - Conductive deafness is the main presentation of:
a. Furunculosis of the external auditory canal.
b. Ear wax.
c. Haematoma auris.
d. Non of the above. - Unilateral hearing loss with pulsating tinnitus is suggestive of:
a. Otosclerosis.
b. Extradural abscess complicating CSOM.
c. Glomus tumor.
d. Acoustic neuroma. - The intracranial complications of cholesteatoma are all of the following EXCEPT:
a. Extradural abscess.
b. Lateral sinus thrombosis.
c. Petrositis.
d. Meningitis. - The most common vertigo is:
a. Acoustic neuroma.
b. Ototoxicity.
c. Meniere’s disease.
d. Benign paroxysmal positional vertigo. - A case of ear infection followed by headache, blurring of vision & vomiting is
suggestive of:
a. Mastoiditis.
b. Petrositis.
c. Labyrinthitis.
d. Brain abscess. - The commonest organism in malignant otitis externa:
a. Streptococci.
b. Pneumococci.
c. Pseudomonas aeroginosa.
d. Moraxella catarrhalis.
All team “One vision … One Mission” 9 - The medial wall of the middle ear shows the following EXCEPT:
a. The oval window.
b. The promontory.
c. The pyramid.
d. The lateral semicircular canal. - Mixed hearing loss may be caused by one of the following:
a. Otosclerosis.
b. Meniere’s disease.
c. Ear wax.
d. Acoustic neuroma. - Pulsating ear discharge may be found in:
a. Extradural abscess.
b. Acute exacerbation of CSOM.
c. Acute otitis media with small perforation.
d. All of the above. - The following are tests of hearing sensitivity EXCEPT:
a. Tuning fork tests.
b. Tympanometry.
c. Auditory Brain stem Response.
d. Pure tone audiometry. - All are true about the Eustachian tube EXCEPT:
a. It opens during swallowing.
b. It ventilates the middle ear.
c. It is wider & horizontal in children.
d. It opens in the oropharynx. - The triad of ear discharge, retro-orbital pain % 6th nerve paralysis is due to:
a. Mastoiditis.
b. Labyrinthitis.
c. Apical petrositis.
d. Lateral sinus thrombosis. - In case of Meniere’s disease with mild SNHL is treated by all the following EXCEPT:
a. Medical treatment.
b. Labyrinthectomy.
c. Endolymphatic sac decompression.
d. Vestibular nerve section. - Fluctuant SNHL usually occurs in:
a. Presbyacusis.
b. Meniere’s disease.
c. Otosclerosis.
d. All of the above.
All team “One vision … One Mission” 10 - Nystagmus & vertigo induced by pressure on the tragus is a sign of:
a. Fistula complicating cholesteatoma.
b. Benign paroxysmal vertigo.
c. Vestibular neuritis.
d. Cholesteatoma only. - Fever, headache, vomiting & neck rigidity in a patient with cholesteatoma is an indication of:
a. Lumbar puncture.
b. CT scan.
c. Fundus examination,
d. All of the above. - Insertion of Grommet tube is indicated in:
a. Acute suppurative otitis media.
b. Secretory otitis media resistant to medical treatment.
c. Chronic otitis media. - Acute mastoiditis is manifested by all of the following EXCEPT:
a. Tenderness over mastoid antrum.
b. Continuous ear discharge.
c. Sagging of postero-superior meatal wall.
d. Obliteration of retro-auricular sulcus. - Fever & rigor developing in a case of cholesteatoma is suggestive of:
a. Cerebellar abscess.
b. Acute mastoiditis.
c. Lateral sinus thrombosis.
d. Labyrinthitis. - Vertigo is a case of cholesteatoma is a suggestive of:
a. Temporal lobe abscess.
b. Acute petrositis.
c. Lateral sinus thrombosis.
d. Labyrinthine fistula. - Equilibrium during angular “rotational” movement is the function of:
a. The utricle.
b. The saccule.
c. The cochlea.
d. The semicircular canal. - The earliest symptom in a case with cholesteatoma that indicates intracranial complication is:
a. Persistent headache.
b. Facial palsy.
c. SNHL.
d. Squint.
All team “One vision … One Mission” 11 - Facial palsy is most commonly:
a. Neoplastic.
b. Traumatic.
c. Herpetic.
d. Bell’s palsy. - Slowly progressive conductive deafness in middle aged female with normal drum & Eustachian tube function is most probably due to:
a. Otitis media with effusion.
b. Otosclerosis.
c. Malingering.
d. Tympanosclerosis. - Adhesive otitis media is a complication of:
a. Cholesteatoma.
b. Otitis media with effusion.
c. Both of them.
d. Non of them. - Following ear surgery, LMNL facial palsy with intact taste sensation of the anterior 2/3 of the tongue indicates injury at the level of:
a. The parotid gland.
b. The internal auditory canal.
c. The stylomastoid foramen.
d. The tympanic segment. - Anesthesia of the face may be caused by:
a. Facial paralysis.
b. Occulomotor paralysis.
c. Trigeminal paralysis.
d. All of the above. - A false +ve fistula test is due to:
a. Labyrinthine fistula with dead ear.
b. Cholesteatoma bridging an inner ear fistula.
c. Hyper mobile footplate of the stapes.
d. All of the above. - The concept that the facial nerve supplies the auricle is related to:
a. Ramsy-Hunt syndrome.
b. Jugular foramen syndrome.
c. Horner’s syndrome.
d. Bell’s palsy. - The most common cause of otitis media with effusion is:
a. Inadequate treatment of acute otitis media.
b. Nasopharyngeal neoplasm.
c. Allergy.
d. Otitic barotraumas.
All team “One vision … One Mission” 12 - Complete LMNL facial paralysis due to acoustic neuroma may be associated by all the following EXCEPT:
a. Loss of lacrimation of the ipsilateral eye.
b. Loss of taste of the anterior 2/3 of the tongue.
c. Loss of stapedial reflex.
d. Hyperacusis. - Topognostic test is used in the assessment of facial paralysis include all the following EXCEPT:
a. Schirmer test.
b. Stapedial reflex.
c. Electroneurography.
d. Gustatory test. - A patient with uncomplicated CSOM has:
a. Ear discharge & headache.
b. Ear discharge & dizziness.
c. Ear discharge & hearing impairment.
d. Ear discharge & fever. - The following drugs are ototoxic:
a. Neomycin.
b. Gramycin.
c. Saliclates.
d. Kanamycin.
e. All of the above.
The Nose - The ostium of the maxillary sinus opens in:
a. Floor of the sinus.
b. Roof of the sinus.
c. Medial wall of the sinus.
d. Between the medial wall & floor of the orbit. - The inferior meatus receives the opening of:
a. The maxillary sinus.
b. The anterior ethmoidal sinus.
c. The posterior ethmoidal sinus.
d. Nasolacrimal duct. - The middle meatus contains:
a. The ostia of the maxillary, anterior ethmoidal & frontal sinuses.
b. The ostia of the posterior ethmoidal sinuses.
c. The nasolacrimal duct. - All are true about rhinoscleroma EXCEPT:
a. It is endemic in Egypt.
b. It is a disease of low immunity & low resistance.
c. It runs in families due to genetic inheritance.
d. It is sub-epithelial inflammatory granuloma.
All team “One vision … One Mission” 13 - Mikulicz cell is a characteristic histological finding in:
a. Rhinoscleroma. b. Rhinosporodosis. c. Aspergillosis.
d. Sarcoidosis. - Russell bodies is a characteristic histological finding in:
a. Rhinoscleroma. b. Rhinosporodosis. c. Aspergillosis.
d. Sarcoidosis. - Perforation of bony part of the nasal septum occurs in:
a. Sarcoidosis.
b. Rhinoscleroma. c. Tuberculosis. d. Syphilis. - Keim test is positive in:
a. Sarcoidosis.
b. Rhinoscleroma. c. Tuberculosis. d. Syphilis. - Spontaneous recovery is usual in:
a. Rhinosporodosis. b. Sarcoidosis.
c. Tuberculosis.
d. Syphilis. - The causative agent of rhinoscleroma is:
a. Sporozoon.
b. Low virulent T.B bacillus.
c. Treponema Ballidum.
d. Gram –ve short capsulated diplobacillus. - Sarcoidosis is:
a. Chronic sub-epithelial inflammatory granuloma of upper respiratory tract.
b. Non caseating granuloma with histological picture similar to T.B.
c. Fungal infection of nasal mucosa.
d. Infection with sporozoon. - The causative agent of lupus vulgaris is:
a. Sporozoon.
b. Low virulent T.B bacillus.
c. Treponema Ballidum.
d. Gram –ve short capsulated diplobacillus.
All team “One vision … One Mission” 14 - Apple-jelly nodules of the nasal mucosa is a clinical finding in:
a. Saroidosis.
b. Rhinoscleroma.
c. Lupus vulgaris.
d. Tuberculosis. - Nasal furunculosis is due to:
a. Staphylococcal infection of a pilosebaceous gland.
b. T.B infection of nasal mucosa.
c. Fungal infection of nasal skin.
d. H.influenza infection of the nose. - F.B of nose is represented by:
a. Bilateral nasal obstruction.
b. Unilateral nasal discharge.
c. Bilateral nasal epistaxis.
d. Unilateral nasal obstruction. - If a patient represented with edema & swelling after nasal trauma:
a. Repair should be done immediately.
b. Repair should be delayed for 3-10 days. - The ideal intranasal decongestant:
a. Must not damage the cilia.
b. Must not be followed by rebound congestion.
c. Must be isotonic & faintly alkaline.
d. All of the above. - The mechanism of nasal allergy is:
a. Type 1 hypersensitivity reaction.
b. Type 2 hypersensitivity reaction.
c. Type 3 hypersensitivity reaction.
d. Type 4 hypersensitivity reaction. - Eosinophils in great numbers in nasal secretion is a finding in:
a. Atrophic rhinitis.
b. Chronic rhinitis.
c. Allergic rhinitis.
d. Acute rhinitis. - The most common type of nasal polypi is:
a. Allergic.
b. Infective.
c. Secondary to malignancy in the nose. - The allergic nasal polyp is:
a. Soft & mobile.
b. Rigid & non mobile.
c. Reddish in color.
d. Grayish in color.
All team “One vision … One Mission” 15 - Sneezing is a prominent feature in:
a. Atrophic rhinitis.
b. Chronic rhinitis.
c. Allergic rhinitis.
d. Acute rhinitis. - Watery nasal discharge is a finding in:
a. Atrophic rhinitis.
b. Allergic rhinitis.
c. Chronic rhinitis.
d. CSF rhinorrhea. - All the following lines of treatment could be applied in rhinoscleroma EXCEPT:
a. Rifampicin.
b. Cytotoxic drugs.
c. Surgery to canalize the stenosed canal.
d. Laser surgery. - Unilateral polypoidal mass arising from the lateral wall of the nose in 55 years old man is most probably:
a. Inverted papilloma.
b. Rhinoscleroma.
c. Allergic nasal polyp.
d. Antrochoanal polyp. - Anterior ethmoid presents bulge in the middle meatus called:
a. Bulla ethmoidalis.
b. Concha bullosa.
c. Lamina papyracea.
d. Haitaus semilunaris. - The most common site of origin of allergic nasal polpi is:
a. Maxillary sinus.
b. Ethmoidal sinus.
c. Frontal sinus.
d. Sphenoid sinus. - CSF rhinorrea is characterized by all of the following EXCEPT:
a. Clear color.
b. Sediment formation after standing in a test tube.
c. Containing glucose.
d. Accelerated flow rate with straining. - All are true about the treatment of CSF rhinorrhea EXCEPT:
a. Antibiotics to avoid infection.
b. Nasal drops.
c. Treatment of the cause.
d. Cleaning & sterilization of the skin of the nasal vestibule.
All team “One vision … One Mission” 16 - Perforation of the cartilaginous part of the nasal septum may be due to:
a. Lupus. b. Leprosy. c. T.B.
d. Syphilis. - Perforation of the bony part of the nasal septum may be due to:
a. Lupus. b. Leprosy. c. T.B.
d. Syphilis. - Radiological finding of sinusitis include all of the following EXCEPT:
a. Bone destruction.
b. Opacity of the affected sinus.
c. Fluid level.
d. Mucosal thickening. - Unilateral chronic maxillary sinusitis is usually of:
a. Nasal origin.
b. Dental origin.
c. Orbital origin.
d. All of the above. - The main presenting symptom of ethmoidal nasal polyp are all of the following EXCEPT:
a. Attack of severe epistaxis.
b. Persistant nasal obstruction.
c. Rhinorrhea.
d. All of the above. - Which of the following is used to confirm nasal allergy:
a. Esinophilia in nasal secretion.
b. Esinophilia in blood.
c. Elevated serum IGE.
d. All of the above. - Nasal regurgitation occurs in all of the following EXCEPT:
a. Ethmoid carcinoma.
b. Palatal paralysis.
c. Advanced maxillary sinus carcinoma.
d. Cleft palate. - Post nasal discharge may occurs:
a. At puberty.
b. At pregnancy.
c. In diabetes.
d. All of the above.
All team “One vision … One Mission” 17 - Post nasal discharge may occurs in:
a. Adenoid abscess.
b. Acute & chronic sinusitis.
c. Non of them.
d. All of them. - Unilateral nasal obstruction in newly born infant may be due to:
a. Antrochoanal polyp.
b. Allergic nasal polyp.
c. Choanal atresia.
d. Non of the above. - Unilateral mucopurulent & purulent nasal discharge may be due to:
a. Unilateral sinusitis.
b. FB in the nose.
c. Non of them.
d. All of them. - The frontal mucocele may be caused by:
a. Chronic frontal sinusitis.
b. Obstruction of a duct of a mucus gland.
c. All of the above. - The following are some general causes of epistaxis EXCEPT:
a. Anemia.
b. Arterial hypertension.
c. Nasopharyngeal angiofibroma.
d. Renal failure. - The most common site of nasal bleeding is:
a. Little’s area.
b. Mac ewing triangle.
c. Pyriform fossa.
d. Sphenoethmoidal recess. - Rhinoscleroma characterized by the following EXCEPT:
a. Hard-like nodules.
b. Histopathology shows Mikulicz cells.
c. Responses to rifampicin.
d. Ulceration of the surrounding tissue. - Resistant epistaxis from below the middle turbinate requires ligation of:
a. The anterior ethmoidal artery.
b. The sphenopalatine artery.
c. The maxillary artery.
d. The internal jugular vein. - Little’s area is the site of anastomosis of the following arteries EXCEPT:
a. Anterior ethmoidal artery.
b. Sphenopalatine artery.
c. Greater palatine artery.
d. Ascending pharyngeal artery.
All team “One vision … One Mission” 18 - Nasopharyngeal carcinoma cause Horner’s syndrome as a result of infiltration of:
a. 3rd cranial nerve.
b. 5th cranial nerve.
c. 7th cranial nerve.
d. Cervical sympathetic chain. - The following drugs can cause epistaxis EXCEPT:
a. Salicylates.
b. Anticoagulants. c. Quinine.
d. Ampicllin. - Periodic headache is a characteristic symptoms in:
a. Frontal sinusitis.
b. Ethmoidal sinusitis.
c. Maxillary sinusitis.
d. Non of the above. - The following lesions may leads to proptosis EXCEPT:
a. Nasopharyngeal angiofibroma.
b. Nasopharyngeal carcinoma.
c. Adenoid hypertrophy,
d. Nasopharyngeal sarcoma. - The following are cranial complications of sinusitis EXCEPT:
a. Osteomylitis of the maxillary & frontal bone.
b. Fistula formation.
c. Subperiosteal abscess.
d. Extradural abscess. - The commonest cause of nasal polypi is:
a. Infective.
b. Malignant.
c. Secondary to malignancy. d. Allergic. - The commonest cause of CSF rhinorrhea is:
a. Congenital. b. Traumatic. c. Infective. d. Neoplastic. - The commonest complication of sinusitis is:
a. Meningitis.
b. Orbital.
c. Extradural abscess.
d. Brain abscess.
All team “One vision … One Mission” 19 - Alternating nasal obstruction is mainly:
a. Allergic.
b. Infective.
c. Neoplastic.
d. Non of them. - Cyclic asphyxia is the presenting symptom is:
a. Bilateral choanal atresia.
b. Adenoids.
c. Acute laryngitis.
d. Nasal allergy. - The main manifestation of antrochoanal polyp is:
a. Proptosis.
b. Unilateral nasal obstruction.
c. Headache.
d. Sneezing. - The commonest cause of epistaxis in 50 years old man is:
a. Hypertension.
b. Angiofibroma.
c. Allergic nasal polypi.
d. Antrochoanal polyp. - Non symptomatic deviated nasal septum needs:
a. Septoplasty.
b. No treatment.
c. Sub-mucperichondrial resection.
d. Cauterization. - The following is complication of SMR of deviated nasal septum:
a. Septal haematoma.
b. Septal abscess.
c. Septal perforation.
d. All of the above. - Headache in sinusitis is due to:
a. Tension headache.
b. Vacuum headache.
c. Toxic headache.
d. All of the above. - The time of occurrence of headache in frontal sinusitis:
a. All the day.
b. At night.
c. Periodic.
d. Non of them.
All team “One vision … One Mission” 20 - Chronic sinusitis has:
a. Low grade fever.
b. Intermittent fever.
c. Remittent fever.
d. No fever. - The point of tenderness in acute frontal sinusitis is:
a. The inner canthus.
b. The supra-orbital margin.
c. The infra-orbital margin.
d. Non of them. - The point of tenderness in acute ethmoidal sinusitis is:
a. The inner canthus.
b. The supra-orbital margin.
c. The infra-orbital margin.
d. Non of them. - The point of tenderness in acute maxillary sinusitis is:
a. The inner canthus.
b. The supra-orbital margin.
c. The infra-orbital margin.
d. Non of them. - Unilateral nasal discharge and unilateral nasal obstruction in 13 years old boy is most probably diagnostic of:
a. Choanal atresia.
b. Adenoids.
c. Nasopharyngeal carcinoma.
d. Non of them. - In frontal sinusitis, the discharge is in:
a. The anterior part of the middle meatus.
b. The posterior part of the middle meatus.
c. All over the middle meatus.
d. The inferior meatus. - In ethmoidal sinusitis, the discharge is in:
a. The anterior part of the middle meatus.
b. The posterior part of the middle meatus.
c. All over the middle meatus.
d. The inferior meatus. - In maxillary sinusitis, the discharge is in:
a. The anterior part of the middle meatus.
b. The posterior part of the middle meatus.
c. All over the middle meatus.
d. The inferior meatus.
All team “One vision … One Mission” 21 - The nasolacrimal duct opens in:
a. Superior meatus.
b. Middle meatus.
c. Inferior meatus.
d. Non of them. - Watery fluid in the maxillary sinus indicates:
a. Suppurative inflammation with irreversible mucosal damage.
b. Suppurative inflammation with reversible pathology.
c. Allergic sinusitis.
d. Catarrhal inflammation. - Mucoid fluid in the maxillary sinus indicates:
a. Suppurative inflammation with irreversible mucosal damage.
b. Suppurative inflammation with reversible pathology.
c. Allergic sinusitis.
d. Catarrhal inflammation. - Mucopurulent fluid in the maxillary sinus indicates:
a. Suppurative inflammation with irreversible mucosal damage.
b. Suppurative inflammation with reversible pathology.
c. Allergic sinusitis.
d. Catarrhal inflammation. - Purulent fluid in the maxillary sinus indicates:
a. Suppurative inflammation with irreversible mucosal damage.
b. Suppurative inflammation with reversible pathology.
c. Allergic sinusitis.
d. Catarrhal inflammation. - Headache may be due to:
a. Eye origin.
b. Dental origin.
c. Non of them.
d. All of them. - Headache may be due to:
a. Sinus origin.
b. Cervical origin.
c. Non of the above.
d. All of the above. - Headache may be due to:
a. Temporal arteritis.
b. Neurogenic origin.
c. Non of them.
d. All of them.
All team “One vision … One Mission” 22 - Headache may be due to:
a. Psycogenic.
b. Allergic origin.
c. Non of them.
d. All of the above. - Headache may be due to:
a. Constipation.
b. Hypotension.
c. Non of the above.
d. All of the above. - Headache may be due to:
a. Anemia.
b. Premenstrual.
c. Hypoglycemia.
d. All of the above. - FB in the nose may be characterized by:
a. Unilateral nasal discharge.
b. Unilateral obstruction.
c. Unilateral epistaxis.
d. All of the above.
The pharynx - The cause of secondary hemorrhage is:
a. Wound sepsis.
b. Unprepared patient.
c. Injury of the pharyngeal muscle.
d. Rising of blood pressure with slipping ligature. - The cause of reactionary hemorrhage is:
a. Wound sepsis.
b. Unprepared patient.
c. Injury of the pharyngeal muscle.
d. Rising of blood pressure with slipping ligature. - The cause of primary hemorrhage is:
a. Wound sepsis.
b. Unprepared patient.
c. Injury of the pharyngeal muscle.
d. Rising of blood pressure with slipping ligature. - Fever in diphtheria is:
a. High grade fever.
b. Low grade fever.
c. Remittent fever.
d. Intermittent fever.
All team “One vision … One Mission” 23 - the pulse in diphtheria is:
a. Weak rapid pulse.
b. Full bounding pulse.
c. Synchronous with the temperature.
d. Non synchronous with the temperature. - In a case of 5 years old boy with a membranous faucial lesion , temp 38° & pulse 180/min, the most probable diagnosis is:
a. Infectious mononucleosis.
b. Acute follicular tonsillitis.
c. Diphtheria.
d. Agranulocytosis. - The causative agent of vincent`s agent:
a. Boreli vencenti.
b. Candida albicans.
c. Barr-epestin virus.
d. Streptococci. - The causative agent of infectious mononucleosis:
a. Boreli vencenti.
b. Candida albicans.
c. Barr-epestin virus.
d. Streptococci. - The causative agent of thrush stomatitis is:
a. Boreli vencenti.
b. Candida albicans.
c. Barr-epestin virus.
d. Streptococci. - Membranous tonsillitis may be due to :
a. Diphtheria.
b. Acute follicular tonsillitis.
c. Infectious mononucleosis.
d. All of the above. - Paul-bunnell test is diagnostic for:
a. Diphtheria.
b. Acute follicular tonsillitis.
c. Infectious mononucleosis.
d. Thrush stomatitis. - Pharyngeal ulcer may be due to:
a. Herpes simplex.
b. Herpes zoster.
c. TB.
d. All of the above.
All team “One vision … One Mission” 24 - Pharyngeal ulcer may be due to:
a. Syphilis.
b. Behcet’s syndrome.
c. AIDS.
d. All of the above. - Pharyngeal ulcer may be due to:
a. Blood diseases.
b. Skin diseases (linchen planus).
c. Toxic (heavy metals).
d. All of the above. - Leucoplakia of the oral & pharyngeal mucosa is:
a. Malignant condition.
b. Precancerous condition.
c. Inflammatory condition.
d. Toxic condition. - The following antibiotic is contraindicated in infectious mononucleosis :
a. Ampicillin.
b. Erythromycin.
c. Cephalosporin.
d. Non of the above. - Adenoid hypertrophy may lead to all of the following EXCEPT:
a. Adenoid face.
b. Otitis media with effusion.
c. Sensory neural deafness.
d. Night mares. - Acute tonsillitis may cause all of the following EXCEPT:
a. Acute retropharyngeal abscess.
b. Chronic retropharyngeal abscess.
c. Para Pharyngeal abscess.
d. Quinsy. - Chronic retropharyngeal abscess is treated by:
a. External drainage posterior to sternomastoid.
b. External drainage anterior to sternomastoid.
c. Internal drainage via longitudinal incision.
d. Non of the above. - Acute retropharyngeal abscess is treated by:
a. External drainage posterior to sternomastoid.
b. External drainage anterior to sternomastoid.
c. Internal drainage via longitudinal incision.
d. Non of the above. - Chronic retropharyngeal abscess is caused by:
a. TB of bodies of the cervical vertebrae.
b. Suppuration of the retropharyngeal gland.
c. Diphtheria bacilli.
d. Non of the above.
All team “One vision … One Mission” 25 - Acute retropharyngeal abscess is caused by:
a. TB of bodies of the cervical vertebrae.
b. Suppuration of the retropharyngeal gland.
c. Diphtheria bacilli.
d. Non of the above. - Frog face appearance, is a clinical manifestation of:
a. Ludwig’s angina.
b. Juvenile nasopharyngeal angiofibroma.
c. Retropharyngeal abscess.
d. Non of the above. - the possible cause of death in case of juvenile nasopharyngeal angiofibroma is:
a. Recurrent infection.
b. Sever epistaxis.
c. Upper respiratory tract obstruction.
d. Non of the above. - Juvenile nasopharyngeal angiofibroma spread to the surrounding tissue because it is:
a. Malignant.
b. Non capsulated.
c. Pre-malignant.
d. Highly vascular. - The cause of bleeding in cases of juvenile nasopharyngeal angiofibroma is:
a. Soft friable tissue.
b. Non muscle coated blood vessels.
c. Non capsulated.
d. Malignancy. - Juvenile nasopharyngeal angiofibroma may cause:
a. Conductive deafness.
b. Sensory neural deafness.
c. Mixed deafness.
d. All of the above. - Ludwig’s angina is:
a. Cellulitis of the pyriform fossa.
b. Cellulitis in the parapharyngeal space.
c. Cellulitis in the retropharyngeal space.
d. Cellulitis of the floor of the mouth. - The most dangerous complication of ludwig`s angina is:
a. Acute laryngeal edema.
b. CHL.
c. Bleeding.
d. Nasal obstruction.
All team “One vision … One Mission” 26 - The swelling in acute retropharyngeal abcess is:
a. In the middle line.
b. Lateral to the middle line.
c. Appears from outside the neck.
d. Non of the above. - The most common site of quinsy is:
a. Superior to tonsils.
b. Lateral to tonsils.
c. Posterior to tonsils.
d. Inferior to the tonsils. - Chordoma is:
a. Malignant tumor.
b. Locally malignant tumor.
c. Benign tumor.
d. Non of the above. - Trotter’s syndrome occurs in:
a. Nasopharyngeal carcinoma.
b. Oropharyngeal carcinoma.
c. Hypopharyngeal carcinoma.
d. Postcricoid carcinoma. - 6th nerve paralysis occurs in the following cases EXCEPT:
a. Nasopharyngeal carcinoma.
b. Cavernous sinus thrombosis.
c. Postcricoid carcinoma.
d. Petrositis. - Tonsillectomy is indicated in all of the following EXCEPT:
a. Blood diseases.
b. Diphtheria carrier.
c. Chronic tonsillitis.
d. Impacted FB. - Tonsillectomy is indicated in all of the following EXCEPT:
a. During epidemic of polio.
b. Tumors of tonsils.
c. After peritonsillar abscess.
d. Symptoms of septic focus. - Tonsillectomy is contraindicated in all of the following EXCEPT:
a. During epidemic of polio.
b. During acute attack.
c. Malignant hypertension.
d. Diphtheria carrier. - Tonsillectomy is contraindicated in all of the following EXCEPT:
a. During menses.
b. Uncontrolled diabetes.
c. After peritonsillar abscess.
d. Full stomach.
All team “One vision … One Mission” 27 - Pain in the ear in cases of acute tonsillitis or following tonsellictomy is referred via:
a. 5th nerve. b. 9th nerve. c. 10th nerve. d. 12th nerve. - Hemorrhage within the 24 hours following tonsillectomy:
a. Primary.
b. Reactionary.
c. Secondary.
d. Non of the above. - Hemorrhage during the operation of tonsillectomy is:
a. Primary.
b. Reactionary.
c. Secondary.
d. Non of the above. - Hemorrhage 7 days following tonsillectomy operation is:
a. Primary.
b. Reactionary.
c. Secondary.
d. Non of the above. - The cause of reactionary hemorrhage after tonsillectomy:
a. Secondary infection.
b. Rising blood pr with slipping of ligature.
c. Injury of the pharyngeal muscles & mucosa.
d. Non of the above. - The cause of secondary hemorrhage after tonsillectomy :
a. Secondary infection.
b. Rising blood pr with slipping of ligature.
c. Injury of the pharyngeal muscles & mucosa.
d. Non of the above. - The cause of suffocation & laryngeal spasm after tonsillectomy:
a. Backward of the tongue.
b. Inhalation of vomitus or blood clots.
c. Extubation spasm.
d. All of the above. - The value of post-tonsillectomy position is:
a. To prevent backward falling of tongue.
b. To prevent inhalation of the vomitus or blood.
c. To detect bleeding.
d. All of the above.
All team “One vision … One Mission” 28 - Acute laryngeal abscess is characterized by all of the following EXCEPT:
a. Occur most commonly in infants.
b. Involves the prevertebral space.
c. Usually occurs with TB of the cervical vertebra.
d. Is seen in lateral X-ray of neck. - Infection reaching the submental & submandibular space is called:
a. Vincent angina.
b. Ludwig’s tumor.
c. Submandibular sialadenitis.
d. Bezold’s abscess. - Vincent angina is characterized by :
a. Very sever systemic symptoms & mild local symptoms.
b. Very sever local symptoms & mild systemic symptoms.
c. Very sever local & systemic symptoms.
d. Very mild local & systemic symptoms. - Contraindication of tonsillectomy includes all of the following EXCEPT:
a. Hemophilia.
b. Acute attack.
c. One attack of quinsy 2 months ago.
d. Active rheumatic arthritis. - Behcet’s disease is characterized by a all of the following EXCEPT:
a. Stomatitis, herps like lesion.
b. Conjunctivitis, corneal opacity, irridocyclitis.
c. Genital ulcer.
d. SNHL.
e. Tendency to recur. - Treatment of Behcet’s disease consist of:
a. Corticosteroids locally & systemic.
b. Cytotoxic drugs.
c. Antihistaminic.
d. Non of them. - Stomatitis associated with skin lesions:
a. Pemphigus.
b. Linchen planus.
c. Lupus erthromatosis.
d. All of the above. - The following metabolic disorder associated with stomatitis:
a. Uremia.
b. DM.
c. Liver disease.
d. All of the above.
All team “One vision … One Mission” 29 - The following are submental swelling EXCEPT:
a. Submental LN.
b. Plunging ranula.
c. Suprahyoid thyroglossal cyst.
d. Cystic hygroma. - The following are midline swelling EXCEPT:
a. Thyroglossal duct cyst.
b. Thyroid isthmus nodule.
c. Dermoid cyst.
d. Pharyngeal pouch. - The following are lateral swelling in neck EXCEPT:
a. Branchial cleft cyst.
b. Carotid body tumor.
c. Lymph gland enlargement.
d. Dermoid cyst. - The following are swelling of the floor of the mouth EXCEPT:
a. Ranula.
b. Dermoid cyst.
c. Tumor of the sublingual salivary gland.
d. Cystic hygroma. - The following signs of pus collection in quinsy:
a. Pain become throbbing.
b. Fever may become hectic.
c. Softening & fluctuation can be detected.
d. All of them. - BULL NECK is known to occur in :
a. Tonsillar diphtheria.
b. Quinsy.
c. Acute tonsillitis.
d. Chronic tonsillitis. - Low grad fever is known to occur in:
a. Tonsillar diphtheria.
b. Quinsy.
c. Acute tonsillitis.
d. Chronic tonsillitis. - Feeble very rapid pulse is known to occur in:
a. Tonsillar diphtheria.
b. Quinsy.
c. Acute tonsillitis.
d. Chronic tonsillitis.
All team “One vision … One Mission” 30
The Oesophagus
- The dysphagia in plummer-vinson syndrome start to:
a. Solids then to fluids.
b. Fluids then to solids.
c. Fluid & solids at the same time.
d. All of the above. - The dysphagia in cardiac achalasia starts to:
a. Solids then to fluids.
b. Fluids then to solids.
c. Fluid & solids at the same time.
d. All of the above. - Plummer-Vinson syndrome is:
a. Malignant condition.
b. Pre-malignant.
c. Locally malignant.
d. Non of the above. - Plummer-Vinson syndrome predispose to:
a. Postcricoid carcinoma.
b. Cancer larynx.
c. Cancer oesophagus.
d. Non of the above. - The anemia in Plummer Vinson syndrome is:
a. Microcytic hypochromic.
b. Macrocytic.
c. Both.
d. Non of them. - X-ray barium swallow showing tea-pot appearance is a finding in:
a. Plummer Vinson syndrome.
b. Cardiac achalasia.
c. Pharyngeal pouch.
d. Cancer oesophagus. - X-ray barium swallow showing rat-tail appearance is a finding in:
a. Corrosive oesophagitis.
b. Cardiac achalasia.
c. Pharyngeal pouch.
d. Cancer oesophagus. - X-ray barium swallow showing parrot-peak appearance is a finding in:
a. Plummer Vinson syndrome.
b. Cardiac achalasia.
c. Pharyngeal pouch.
d. Cancer oesophagus.
All team “One vision … One Mission” 31 - Dysphagia in cancer oesophagus is :
a. Progressive. b. Regressive. c. Stationary. d. Intermittent. - Dysphagia in cardiac achalasia is:
a. Progressive. b. Regressive. c. Stationary. d. Intermittent. - Dysphagia lusoria is:
a. Compression of the oesophagus by abnormally located RT subclavian artery or double aorta.
b. Herniation of the pharyngeal mucosa via kllian dehiscence.
c. Chronic superficial oesophagitis with web formation.
d. Failure of relaxation of cardic sphincter. - PATRESON-BROWN-KELLY syndrome is:
a. Compression of the oesophagus by abnormally located RT subclavian artery or double aorta.
b. Herniation of the pharyngeal mucosa via kllian dehiscence.
c. Chronic superficial oesophagitis with web formation.
d. Failure of relaxation of cardic sphincter. - Cardiac achalasia is:
a. Compression of the oesophagus by abnormally located RT subclavian artery or double aorta.
b. Herniation of the pharyngeal mucosa via kllian dehiscence.
c. Chronic superficial oesophagitis with web formation.
d. Failure of relaxation of cardic sphincter. - The cause of death in corrosive oesphagitis may be:
a. Dehydration due to electrolytes imbalance.
b. Stridor due to laryngeal oedema.
c. Both of them.
d. Non of them. - X-ray with barium swallow showing multiple stricture in the oesophagus ia a diagnostic finding in:
a. Chronic corrosive oesophagitis.
b. Cardiac achalasia.
c. Plummer Vinson syndrome.
d. Non of them. - Failure of relaxation of crico-pharyngeal sphincter during swallowing leads to:
a. Plummer Vinson syndrome.
b. Cardiac achalasia.
c. Pharyngeal pouch.
d. Cancer oesophagus.
All team “One vision … One Mission” 32 - Pharyngeal pouch occurs mostly in:
a. Old males.
b. Old females.
c. Infants.
d. Adult males. - All are correct about corrosive oesophaditis EXCEPT:
a. Shock may occur due to electrolytes imbalance.
b. Normal feeding is encouraged.
c. Vomiting is not encouraged.
d. Cortisone in the acute stage is contraindicated. - Dysphagia may be due to:
a. Aneurysm of the aorta.
b. Enlarged left atrium.
c. Mediastinal tumor.
d. All of the above. - Dysphagia may be due to:
a. Aneurysm of the ICA.
b. Enlarged thyroid.
c. Enlarged malignant gland.
d. All of the above. - Violent vomiting or large meal may cause:
a. Pharyngeal pouch.
b. Cardiac achalasia.
c. Spontaneous rupture of the oesophagus.
d. Plummer Vinson syndrome.
The Larynx, Trachea & Bronchi - Apnea immediately after opening the trachea is due to:
a. Rise of the blood carbon dioxide level.
b. Rise of the blood O2 level.
c. Wash of the blood carbon dioxide level.
d. Non of the above. - Which is true about laryngeal carcinoma:
a. Commoner in males.
b. The commonest type is squamous cell carcinoma.
c. Is predisposed by smoking.
d. All of the above. - Inhaled smooth small FB is commonly arrested in:
a. The larynx.
b. The trachea.
c. The right bronchus.
d. The left bronchus.
All team “One vision … One Mission” 33 - 30 years old female suffring form bilateral nasal obstruction, crusty nose, hoarseness of voice & stridor. The most probable cause is:
a. Allergic rhinitis.
b. Vasomotor rhinitis.
c. Rhino laryngo scleroma.
d. Acute rhinosinusitis. - The left recurrent laryngeal nerve swing in the chest around:
a. Aortic arch.
b. Left main bronchus.
c. Left ventricle.
d. Thoracic duct. - The commonest cause of breathing difficulty after tracheostomy is:
a. Pneumonia.
b. Obstruction of the tube by secretion.
c. Surgical emphysema.
d. Pneumothorax. - Laryngeal lesions are investigated by:
a. CT.
b. MRI.
c. Endoscopy & biopsy.
d. All of the above. - Singer’s nodules:
a. Localized epithelial hyperkeratosis on the free edge of the vocal cord.
b. Premalignant nodules.
c. Chronic infectious granuloma.
d. Allergic nodules. - The site of singer`s nodules is:
a. At the epiglottis.
b. At the junction of the anterior 1/3 with posterior 2/3 of the vocal cords.
c. At the arytenoids.
d. Non of the above. - Leucoplakia of the larynx is:
a. Epithelial hyperplasia.
b. Epithelial hypertrophy.
c. Epithelial degeneration.
d. Non of the above. - The causative agent of acute laryngo-tracheal bronchitis is:
a. Pneumococci.
b. Staphylococci.
c. Streptococcus haemolyticus.
d. Non of the above.
All team “One vision … One Mission” 34 - TB of the larynx affects:
a. The posterior part.
b. The middle part.
c. The anterior part.
d. The subglottic part. - Scleroma of the larynx affects:
a. The posterior part.
b. The middle part.
c. The anterior part.
d. The subglottic part. - Syphilis of the larynx affects:
a. The posterior part.
b. The middle part.
c. The anterior part.
d. The subglottic part. - Painful cough & dysphagia occur in:
a. Syphilis of larynx.
b. Scleroma of the larynx.
c. TB of the larynx.
d. Lupus of the larynx. - Single laryngeal papilloma is:
a. Locally malignant lesion.
b. Malignant lesion.
c. Precancerous.
d. Non of the above. - Single laryngeal papilloma occurs in:
a. Adults.
b. Children.
c. Both of them.
d. Non of them. - Multiple laryngeal papilloma occurs in:
a. Adults.
b. Children.
c. Both of them.
d. Non of them. - The following conditions cause stridor EXCEPT:
a. Laryngeal diphtheria.
b. Acute laryngitis in adult.
c. Acute laryngitis in children.
d. Multiple laryngeal papilloma. - The following conditions cause stridor EXCEPT:
a. Acute epiglottitis.
b. Bilateral abductor paralysis.
c. Bilateral adductor paralysis.
d. Laryngoscleroma.
All team “One vision … One Mission” 35 - A newborn with cyanosis and respiratory difficulty improved by insertion of an oral airway. The most probable diagnosis is:
a. Laryngomalacia.
b. Congenital laryngeal web.
c. Congenital subglottic stenosis.
d. Congenital bilateral choanal atresia. - The narrowest part in the infantile larynx is:
a. The supraglottic area.
b. The subglottic area.
c. The pyriform fossa.
d. Non of the above. - Cyclic asphyxia is a manifestation of:
a. Congenital bilateral choanal atresia.
b. Laryngeal web.
c. Acute laryngitis.
d. Non of the above. - Surgical emphysema after tracheostomy occurs due to:
a. When small tube is used and a wide opening made in the trachea.
b. Injury of the pleura.
c. Non of them.
d. Both of them. - Surgical emphysema after tracheostomy occurs due to:
a. When the skin is closed tightly.
b. Injury of the pleura.
c. Non of them.
d. Both of them. - Mediastinal emphysema after tracheostomy occurs due to:
a. When the pretrachial fascia is sutured tightly.
b. Injury of the pleura.
c. Non of them.
d. Both of them. - Pneumothorax after trachestomy occurs due to:
a. When the pretrachial fascia is sutured tightly.
b. Injury of the pleura.
c. Non of them.
d. Both of them. - The following drug is contraindicated after tracheostomy:
a. Expectorants.
b. Analgesics.
c. Opiates.
d. Non of them.
All team “One vision … One Mission” 36 - The best position after trachestomy:
a. Supine.
b. Semi-sitting.
c. Standing.
d. On one side. - Dyspnea, crepitation and expectoration of large amount of frothy stained sputum after trachestomy is suspected of:
a. Pneumothorax.
b. Acute pulmonary edema.
c. Mediastinal emphysema.
d. Non of them. - The tube may slip due to:
a. Small sized tube.
b. Pulled out by voilent cough.
c. Loosely tied tape.
d. All of the above. - Valvular obstructive emphysema occurs due to:
a. Partial obstruction of the bronchus.
b. Complete obstruction of the bronchus.
c. When the pretrachial fascia is sutured tightly.
d. Injury of the pleura. - Ulceration of the vocal cord edge (mouth nibbled) occurs in:
a. TB.
b. Scleroma. c. Syphilis.
d. Sarcoidosis. - Structures in the larynx responsible for sphincteric function:
a. Vocal cords.
b. Ventricular bands.
c. Aryoepiglottic folds.
d. All of the above. - Laryngeal stenosis may be due to:
a. Scleroma.
b. TB.
c. High tracheostomy.
d. All of the above. - Laryngeal stenosis may be due to:
a. Scleroma.
b. Congenital.
c. Traumatic.
d. All of the above. - Laryngeal stenosis may be due to:
a. Perichondritis.
b. Endotracheal intubation.
c. Syphilis.
d. All of the above.
All team “One vision … One Mission” 37
ThePharynx
1) a. 10)d. 19)a. 28)d. 37)a. 46)d. 55)d.
2) d. 11)c. 20)c. 29)a. 38)d. 47)d. 56)d.
3) c. 12)d. 21)a. 30)a. 39)c. 48)c. 57)d.
4) b. 13)d. 22)b. 31)a. 40)b. 49)b. 58)d.
4) a. 13)d.
5) d. 14)d. 23)b. 32)b. 41)b. 50)b. 59)d.
5) a. 14)c.
6) c. 15)b. 24)b. 33)a. 42)a. 51)c. 60)a.
6) c. 15)a.
7) a. 16)a. 25)b. 34)c. 43)b. 52)d. 61)a.
7) d. 16)a.
7) d. 16)c. 25)a. 34)d.
8) c. 17)c. 26)b. 35)c. 44)b. 53)a. 62)a.
8) b. 17)a.
8) a. 17)a. 26)a. 35)d.
9) b. 18)b. 27)a. 36)a. 45)d. 54)d.
9) a. 18)d.
9) b. 18)b. 27)b. 36)d.
TheOesophagus
1) a. 10)d. 19) d.
2) b. 11)a. 20) d.
3) b. 12)c. 21) d.
TheLarynx,Trachea&Bronchi
1) c. 10)a. 19)b. 28)c. 37) d.
2) d. 11)c. 20)c. 29)b.
3) c. 4) c. 12)a. 13)d. 21)d. 22)b. 30)b. 31)d.
5) a. 14)c. 23)a. 32)a.
6) b. 15)c. 24)a. 33)a.
All team “One vision … One Mission”
39
تم بحمد الله
TheEar
1) a. 9) e. 17)b. 25)c. 33) e. 41)b,d. 49)a. 57)d. 65)b. 73)c. 81)a. 89)d. 97) d.
2) c. 10) b. 18)b. 26)a,c. 34) e. 42)e. 50)a. 58)d. 66)d. 74)a. 82)d. 90)b. 98) c.
3) b.
11) c.
19)a.
27)a,c.
35) a,b. 43)b,d. 44)f. 51)b. 52)d. 59)d. 60)b. 67)b. 68)c. 75)d. 76)b. 83)b. 84)d. 91)b. 92)c. 99) c. 100)
3)
12)b. 13)c. 21)a. 22)c. 30)a,b,c. 31)d. 39)c. 40)d. 48)d. 49)a. 57)b. 58)a. 66)c. 67)a. 75)a. 76)d.
6) a. 14) b. 22)a. 30)d. 38) c. 46)a. 54)d. 62)c. 70)d.
7) a.
15) c.
23)e.
31)e.
39) a,b,d.
47)a.
55)b.
63)c.
71)d.
79)b. 80)b. 87)d. 88)a. 95)a. 96)a.
The Answers
4) c. 12) c. 20)a. 28)c. 36) c,d,e.
5) a.
13) a.
21)c.
29)f.
37) b,c.
45)c.
53)b.
61)d.
69)c.
77)d. 78)c. 85)c. 86)d. 93)c. 94)c.
8) a. 16) a. 24)c. 32)a. 40) c. 48)b. 56)d. 64)b. 72)c.
TheNose 1) d. 2) d.
10)d. 11)b. 19)b,c. 20)a. 28)b. 29)b. 37)d. 38)d. 46)d. 47)d. 55)a. 56)a. 64)b. 65)a. 73)d. 74)b. 82) d.
a. 4) c.
e.
5) a. 14)a. 23)b,d. 32)a. 41)d. 50)c. 59)b. 68)a. 77)d.
6) b. 15)b,d. 24)b. 33)b. 42)c. 51)d. 60)d. 69)c. 78)d.
7) d. 16)b. 25)a. 34)a. 43)a. 52)d. 61)d. 70)b. 79)d.
8) a. 17)d. 26)a. 35)d. 44)d. 53)b. 62)c. 71)c. 80)d.
9) b. 18)a. 27)b. 36)a. 45)b. 54)b. 63)d. 72)c. 81)d.
All team “One vision … One Mission”
38